One second you’re vertical, the next you’re eye-level with your dog’s food bowl. No warning, no pain — just a jarring collapse that makes you wonder if your legs are still taking orders from your brain. It’s not just embarrassing (especially in front of coworkers or family), it’s alarming. Why do your legs suddenly ghost you like a bad Tinder date?
🔎 Top Causes of Sudden Leg Collapse
Why Do My Legs Suddenly Give Out?
It’s not just frustrating — it can be downright scary. One moment you’re walking through the kitchen, the next you’re clinging to the counter like it’s the mast of a sinking ship. If your legs give out and you can’t stand, you’re not alone — and you’re not imagining things either.
Sudden leg weakness or collapse is more common than you’d think. It can stem from temporary issues like dehydration or muscle fatigue, or it can be the red flag of a serious neurological or circulatory disorder. In the U.S. alone, over 200,000 ER visits annually are linked to unexplained leg weakness or falls related to lower limb instability ⧉.
Let’s unpack why your legs might betray you — and what you can do about it.
📉 Risk Factors for Sudden Leg Collapse
Common Causes Behind Sudden Leg Weakness
There are plenty of culprits behind the “why can’t I stand up?” moment. Here are the heavy hitters:
- Muscle cramps or spasms — These involuntary contractions can quite literally drop you to the floor. Often triggered by dehydration, mineral imbalance (magnesium, potassium), or overuse.
- Peripheral neuropathy — Common in diabetics, this condition affects the nerves in the legs and feet, causing numbness, tingling, and instability ⧉.
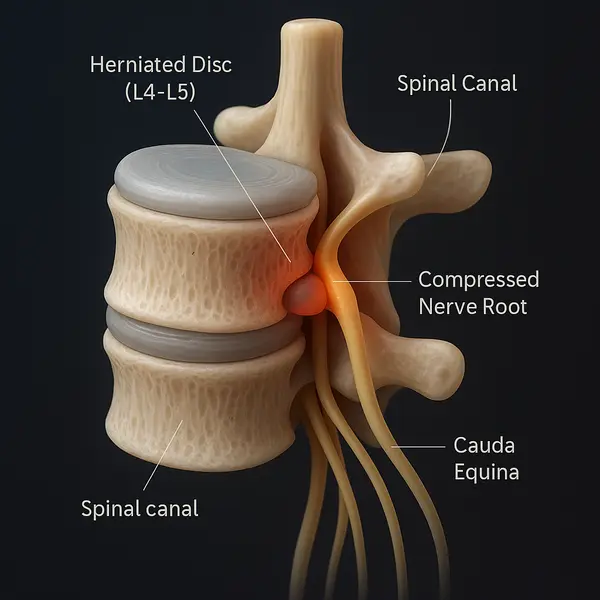
- Radiculopathy or herniated discs — When nerves in the lower spine are compressed, it can result in weakness or a “buckling” sensation in the legs. 📍 Case: A 61-year-old woman presented with sudden bilateral leg weakness and numbness. Imaging revealed severe lumbar radiculopathy due to spinal stenosis. She was unable to walk or stand without support. Surgical decompression restored partial function within six weeks ⧉.
- Transient ischemic attacks (TIAs) or minor strokes — These “mini strokes” can cause temporary motor loss or imbalance without warning.
- Multiple sclerosis (MS) — MS often begins with weakness or tingling in the limbs. This autoimmune disease affects over 900,000 Americans ⧉.
- Guillain-Barré syndrome (GBS) — A 41-year-old male arrived with four days of progressive leg pain, edema, and weakness. Neurological testing confirmed GBS. He required IVIG and intensive rehab, but made a full recovery within two months ⧉.
Reyus Mammadli, medical consultant, recommends not ignoring even a one-time episode: “If your legs collapse unexpectedly, think of it as your body’s emergency alert. Don’t snooze it.”
Red Flag Symptoms You Shouldn’t Ignore
Not every case of leg weakness means a trip to the ER — but some symptoms are bright-red warning signs. To help you distinguish between what’s urgent and what’s just annoying, here’s a breakdown of symptoms, what they might indicate, and how to recognize them in real life.
🚨 Primary Red Flags (Seek immediate medical attention)
- Numbness or tingling in the groin or inner thighs (saddle anesthesia): This sensation feels like you’re sitting on a rolled-up towel, and it may indicate cauda equina syndrome, a rare but serious condition involving compression of nerves at the base of the spine. This is a surgical emergency ⧉. 📍 Case: A 48-year-old male experienced growing leg weakness for weeks. Three days before hospital admission, he lost control of his bladder and began having saddle numbness. MRI revealed cauda equina compression requiring emergency surgery ⧉.
- Sudden loss of bladder or bowel control: If this occurs alongside leg weakness or back pain, it’s a high-priority emergency — often tied to spinal cord compression or severe nerve damage.
- One-sided leg weakness with facial drooping, slurred speech, or vision changes: Classic signs of a stroke. These symptoms may last several minutes or hours and usually come on quickly. Call 911 immediately. 📍 Case: A woman collapsed at home and presented with dysarthria and left leg weakness. CT confirmed a minor ischemic stroke in the right hemisphere ⧉.
- Sudden, intense back pain with leg collapse: Could indicate a herniated disc, spinal tumor, or vertebral fracture, especially in older adults or those with osteoporosis.
⚠️ Secondary Symptoms (Still important — consult a physician)
- Leg heaviness or fatigue after short walking distance: May point to peripheral artery disease (PAD) — often described as “walking through wet cement.” 📍 Case: A 70-year-old male reported progressive leg fatigue and cold feet after walking two blocks. Duplex ultrasound showed significant arterial occlusion consistent with PAD ⧉.
- Burning or stabbing pain in the legs and feet: A hallmark of peripheral neuropathy, especially in people with diabetes. Pain often worsens at night.
- Cramping or stiffness that locks the legs temporarily: Often linked to electrolyte imbalances or dehydration. Common in athletes and older adults. 📍 Case: A man experienced recurrent leg cramps and collapses during workouts. Blood work revealed hypokalemia. After potassium correction, symptoms resolved within days ⧉.
- Gradual onset of weakness over weeks or months: Could be due to multiple sclerosis, ALS, or a slow-growing spinal tumor.
- Feeling of instability or imbalance without pain: Might be early signs of Parkinson’s disease or cerebellar disorders.
⏱ Symptom Duration and Progression: What Matters
- Sudden onset (seconds to minutes): Suggests vascular or neurological events (stroke, TIA, herniated disc).
- Fluctuating over hours to days: May indicate autoimmune or inflammatory causes (MS, Guillain-Barré).
- Chronic but worsening over time: Usually degenerative (arthritis, spinal stenosis).
Medical consultant Reyus Mammadli emphasizes: “The symptom itself doesn’t define the disease — the timeline and the context do. Keep a record. It may save you months of misdiagnosis.”
What Doctors Look For: Diagnosing Leg Collapse
Diagnosing sudden leg weakness is like solving a medical mystery. Here’s how doctors approach it:
| Diagnostic Test | What It Checks | Accuracy (1–10) | Avg. U.S. Cost |
|---|---|---|---|
| MRI (Lumbar Spine) | Herniated discs, nerve compression | 9 | $1,200–$3,000 |
| EMG/Nerve Conduction | Nerve function | 8 | $300–$1,500 |
| Blood Panels | Electrolytes, inflammation markers | 7 | $100–$300 |
| Ultrasound (Legs) | Vascular issues like PAD or DVT | 7 | $200–$500 |
Newer diagnostic tools now include AI-assisted MRI analysis, speeding up interpretation time and reducing error rates in spinal pathology ⧉.
Real Cases: When It Happened Out of Nowhere
📍 Austin, TX — A 47-year-old tech worker stood up after a Zoom call and dropped instantly. “It felt like my knees ghosted me,” she joked. Turns out it was a disc herniation compressing her L5 nerve.
📍 Minneapolis, MN — A 62-year-old retired coach collapsed while unloading groceries. Diagnosed with severe diabetic neuropathy and vitamin B12 deficiency. A routine symptom he had ignored for months finally took him down.
📍 Boston, MA — A 15-year-old girl stopped walking after a stressful school incident. All tests were normal. A neurologist diagnosed Functional Neurological Disorder (FND). After therapy and rehab, she returned to full activity in three weeks ⧉.
Latest Treatments and Rehabilitation Options
Treatment should map to the cause. Below is a practical menu of options with plain‑English explanations, typical U.S. costs, complexity, expected timelines, and an effectiveness score (1–10). Where evidence is mixed, it’s said upfront.
Medications
Gabapentin (for neuropathic pain)
- What it is: A nerve‑calming medicine used widely for nerve pain in the legs and feet. Think of it as “noise‑canceling” for over‑firing pain signals. ⧉
- Complexity: Low (oral tablets).
- Effectiveness: 6/10 for many neuropathic pain conditions; not a strength drug, so it won’t fix true motor weakness.
- Typical cost (U.S.): Generic often $7–$30/month with coupons; retail varies. ⧉
- Duration to judge effect: 2–4 weeks at a stable dose.
- Watch‑outs: Drowsiness, dizziness; taper rather than stop abruptly.
Baclofen (for muscle spasticity and painful spasms)
- What it is: A muscle relaxant that reduces spinal reflex overactivity (spasticity) seen after stroke, MS, or spinal cord problems. ⧉
- Complexity: Low (oral) to High (implanted pump).
- Effectiveness: 7/10 oral for spasticity; can be 8–9/10 when delivered intrathecally via a pump in severe cases. ⧉
- Typical cost (U.S.): Generic oral often ~$10/month with coupons. ⧉
- Advanced option: Intrathecal baclofen pump (ITB) — for refractory spasticity; first‑year total care costs reported in studies vary widely (~$27k–$76k median ranges reported). ⧉
- Duration: Oral trial 2–6 weeks; pump trials require a test dose and ongoing refills.
- Watch‑outs: Sedation, weakness (if dose too high); pump requires maintenance and urgent care if it malfunctions.
Corticosteroids
- What they are: Strong anti‑inflammatories. Their role depends on the diagnosis:
- Acute radiculopathy from a herniated disc: short oral steroid tapers can modestly improve function but do not reliably reduce pain. Effectiveness: 4–5/10. ⧉
- MS relapses: high‑dose oral or IV steroids speed recovery from disabling relapses. Effectiveness: 7–8/10 for shortening relapse duration (not a long‑term disease modifier). ⧉
- Typical cost (U.S.): Prednisone generics often $2–$15 for short courses with coupons. ⧉
- Duration: Usually 3–5 days (MS relapse) or a brief taper for back‑related inflammation.
- Watch‑outs: Temporary insomnia, mood changes, blood sugar spikes; avoid frequent repeats without a plan.
Reyus Mammadli, medical consultant, notes: “Pills can quiet symptoms, but the ‘why’ behind the weakness still wins the day. Treat the cause, not just the noise.”
Assistive Devices & Technology
Ankle‑Foot Orthosis (AFO) for foot drop/instability
- What it is: A lightweight brace that prevents toe‑drag and stabilizes the ankle during swing and stance.
- Effectiveness: 7/10 for gait safety and efficiency; improves walking speed and stride in clinical studies. ⧉
- Typical cost (U.S.): Off‑the‑shelf ~$200–$600; custom ~$475–$1,100+ depending on materials and lab. ⧉ ⧉
- Complexity: Low (fitting by an orthotist).
- Duration: Wear daily; reassess fit every 6–12 months.
- Watch‑outs: Skin hotspots; check for redness after each wear.
Robotic exoskeletons / exosuits (clinic or personal use)
- What they are: Powered hip‑knee devices (e.g., ReWalk, Ekso Indego) that enable overground, therapist‑supervised gait training; select models are FDA‑cleared for home use in spinal cord injury. ⧉
- Effectiveness: 6–7/10 as an adjunct to therapy; best early after stroke/SCI and when combined with conventional PT. ⧉ ⧉
- Typical cost (U.S.): Personal devices now have Medicare reimbursement rates ~$82k–$109k; clinics bill standard PT rates per session. ⧉ ⧉
- Complexity: High (screening, training, and therapist supervision).
- Duration: Typically 30–60 min sessions, 2–5×/week during intensive blocks.
- Watch‑outs: Height/weight limits; requires balance and bone health screening.
Therapies
Physical therapy (PT) with gait and strength training
- What it is: A tailored program to build strength, balance, and movement patterns; think “re‑coding” how you stand and walk.
- Effectiveness: 7–9/10 when done consistently; foundational for nearly all causes.
- Typical cost (U.S.): $75–$150 per session self‑pay; specialized programs may run higher. ⧉ ⧉
- Duration: Common starter block is 2–3 sessions/week for 6–8 weeks, then taper.
- Watch‑outs: Progress is rarely linear; adherence (home program) drives outcomes.
TENS (transcutaneous electrical nerve stimulation)
- What it is: Small device that sends a gentle current through the skin to disrupt pain signaling; home use is common.
- Effectiveness: 3–5/10 overall for neuropathic pain — evidence is inconclusive versus sham. ⧉
- Typical cost (U.S.): Units ~$30–$150; electrode pads ~$10–$30 per pack. ⧉ ⧉
- Complexity: Low.
- Duration: 20–30 minutes per session, up to a few times daily.
- Watch‑outs: Avoid if you have a pacemaker or implanted defibrillator unless cleared by your cardiologist.
VR‑based rehabilitation (for balance, gait, and confidence)
- What it is: Virtual‑reality tasks that train stepping, balance, and coordination; turns rehab into a goal‑oriented “game” with measurable scores.
- Effectiveness: 6–8/10 as an adjunct; meta‑analyses show improvements in gait/balance after stroke. ⧉
- Typical cost (U.S.): Usually billed as standard PT/OT visit (see costs above); home headsets cost ~$300–$600 (not medical‑grade).
- Complexity: Low–Moderate (needs supervision for safety).
- Duration: 20–45 minutes per session, 2–3×/week in programs.
📍 Case (rehab focus): A patient with Guillain‑Barré syndrome enrolled in intensive PT augmented by robotic gait training. Over ~8 weeks, they progressed from wheelchair to independent short‑distance ambulation 3×/week — a typical arc when nerves are healing and muscles are re‑trained.
Reyus Mammadli adds: “If you can’t do everything today, do the most important something — early PT, safe bracing, or a short diagnostic sprint. Momentum beats perfection.”
How to Prevent Sudden Leg Weakness
Nobody wants to feel their legs bail mid-step. Here’s how to stay grounded:
- Stay hydrated — Dehydration is a major cause of cramps.
- Balance your electrolytes — Especially magnesium and potassium.
- Watch your blood sugar — Sudden spikes or drops can mess with nerve signals.
- Strengthen your lower body — Simple resistance exercises can do wonders.
- Pay attention to early signs — Numb toes today, collapsed knees tomorrow.
📍 Case: A 40-year-old woman with Charcot-Marie-Tooth disease improved her walking ability by following a six-month strength-training program focused on calves and quads, combined with physical therapy. Her fall rate dropped by 70%. ⧉
📅 5-Day Recovery Plan for Sudden Leg Weakness
Pro Tip: Keep a symptom diary. What time it happened, what you were doing, how long it lasted. It’s gold for your doctor.
Editorial Advice
If your legs gave out once, it might be a fluke. If it happens again — it’s a message. A message from your spine, your nerves, your muscles, or even your brain.
According to medical consultant Reyus Mammadli, “Early intervention is key. What begins as mild weakness could evolve into permanent nerve damage if left unchecked.”
Here’s what you can do today:
- Book a neurological exam if it’s happened more than once
- Add magnesium-rich foods to your meals (hello, spinach!)
- Stretch your calves before bed
- Don’t ignore the weird stuff — your body’s smarter than you think
And remember: if your knees ever ghost you again, you’ll know exactly what to do next time.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.