Left breast pain is discomfort localized to the left side of the chest that may come from breast tissue itself or from nearby structures, a condition doctors often describe as mastalgia. In plain language, it means pain that feels like it’s in the breast, even though the source isn’t always the breast at all. It’s like a fire alarm going off in one room when the smoke is actually coming from the hallway.
Left breast pain that appears on its own is far more likely to be benign than dangerous, especially in women under 50, with studies showing that most cases are related to hormonal fluctuations, fibrocystic breast changes, or musculoskeletal strain. Cyclical mastalgia affects up to 70% of women at some point, while non-cyclical pain can be linked to costochondritis, muscle tension, or nerve irritation. Despite common fears, isolated breast pain without a lump is rarely a sign of breast cancer.
When pain is felt in the left breast area, especially if it comes and goes or changes with movement, hormones, or posture, guessing isn’t helpful. Understanding whether the source is hormonal, structural, or referred pain from the chest wall or heart-adjacent tissues is the key step forward. Breaking down the possible causes, red flags, and next steps makes it easier to decide when reassurance is enough and when further evaluation actually matters.
Hormonal Changes
Left-sided breast pain (mastalgia) is frequently associated with hormonal fluctuations involving estrogen and progesterone. Cyclic mastalgia typically occurs during the luteal phase of the menstrual cycle and may be more noticeable in one breast due to asymmetrical tissue sensitivity. Hormonal changes related to pregnancy, perimenopause, menopause, or the use of oral contraceptives and hormone replacement therapy can also contribute to localized discomfort, tenderness, or a dull aching sensation.
Musculoskeletal Causes
Pain originating from the chest wall is a common non-breast cause of left breast pain. Conditions such as costochondritis (inflammation of the costosternal joints), intercostal muscle strain, rib trauma, or cervical and thoracic spine disorders can refer pain to the left breast area. This type of pain is often sharp or burning, worsens with movement or palpation, and is not related to hormonal cycles.
Breast Conditions
Several benign breast disorders may cause unilateral left breast pain. Fibrocystic breast changes can lead to localized nodularity and tenderness. Breast cysts, duct ectasia, and mastitis (including non-lactational mastitis) may also present with pain, swelling, or warmth. While breast cancer is an uncommon cause of isolated pain without other symptoms, inflammatory breast cancer may present with pain accompanied by skin changes and should always be excluded through proper evaluation.
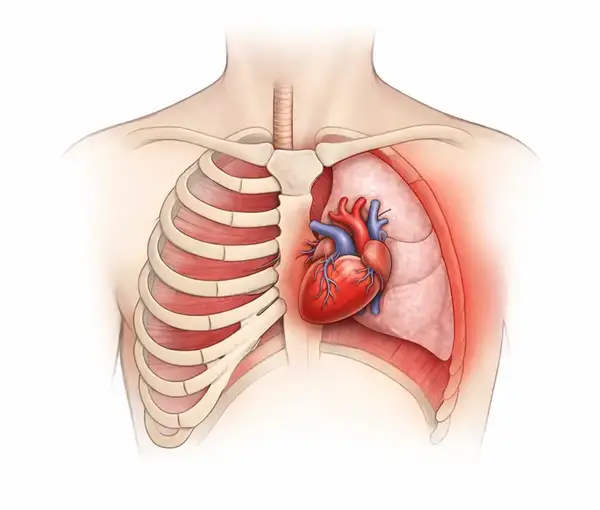
Cardiac-Related Pain
Because the heart is located on the left side of the chest, cardiac conditions must be considered when evaluating left breast pain. Angina pectoris, myocardial ischemia, or pericarditis can produce pain that radiates to the left breast, shoulder, arm, or jaw. Cardiac-related pain is often described as pressure-like or squeezing and may be associated with shortness of breath, diaphoresis, nausea, or dizziness. Such symptoms require immediate medical attention.
Digestive Causes
Gastrointestinal disorders can mimic breast pain. Gastroesophageal reflux disease (GERD), esophageal spasm, and hiatal hernia may cause burning or aching pain behind the left breast. Gastric distension and excessive gas can also produce referred discomfort to the chest and breast region, particularly after meals.
Lung Conditions
Pulmonary and pleural conditions may contribute to left-sided breast pain. Pleuritis, pneumonia involving the left lung, or pulmonary embolism can cause sharp pain that worsens with deep breathing or coughing. These conditions are often accompanied by respiratory symptoms such as cough, fever, or dyspnea and require prompt medical evaluation.
Stress and Anxiety
Psychological factors such as chronic stress, anxiety disorders, and panic attacks can lead to chest wall muscle tension and heightened pain perception. Anxiety-related chest pain may present as tightness or stabbing discomfort in the left breast area and is often accompanied by palpitations, hyperventilation, or a sense of impending doom. Although non-cardiac in origin, cardiac causes must always be ruled out first.
When to Worry
Left breast pain warrants medical attention if it is persistent, progressively worsening, or associated with alarming features such as a palpable mass, nipple discharge, skin dimpling, redness, unexplained weight loss, fever, or systemic symptoms. Sudden severe pain accompanied by cardiac or respiratory symptoms should be treated as a medical emergency.
Medical Evaluation
Clinical evaluation typically includes a detailed medical history, physical examination, and targeted diagnostic testing. Depending on age and risk factors, imaging studies such as mammography, breast ultrasound, or magnetic resonance imaging (MRI) may be indicated. Additional tests, including electrocardiography, chest imaging, or gastrointestinal evaluation, may be required to identify non-breast causes. Accurate diagnosis is essential for appropriate management.
Editorial Advice
Left breast pain has a wide range of potential causes, many of which are benign and treatable. However, self-diagnosis should be avoided, especially when pain is unilateral or recurrent. Timely consultation with a qualified healthcare professional allows for accurate diagnosis, exclusion of serious conditions, and reassurance when appropriate. Paying attention to accompanying symptoms and seeking care early remains the most reliable approach to protecting long-term health.
References
Breast pain (clinical overview) – Mayo Clinic (patient education resource) https://www.mayoclinic.org/
Mastalgia: causes and evaluation – Cleveland Clinic (clinical overview) https://my.clevelandclinic.org/
Chest wall pain and costochondritis – Johns Hopkins Medicine (patient guide) https://www.hopkinsmedicine.org/
Heart-related chest pain symptoms – American Heart Association (cardiology reference) https://www.heart.org/
Gastroesophageal reflux disease overview – National Institute of Diabetes and Digestive and Kidney Diseases (digestive health resource) https://www.niddk.nih.gov/
Pleural and lung-related chest pain – Centers for Disease Control and Prevention (public health information) https://www.cdc.gov/
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.