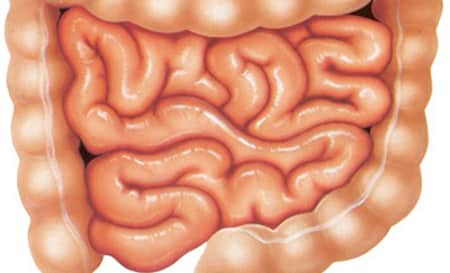
Irritable bowel syndrome (IBS) impacts between 6 – 18% of individuals worldwide. In the article we will consider the main symptoms of this disease.
Irritable bowel syndrome (IBS) is a group of symptoms — including abdominal pain and changes in the pattern of defecation without any proof of underlying damage. These symptoms occur over a long time, frequently years. It has actually been categorized into 4 main types depending upon whether diarrhea is common, constipation prevails, both are common, or neither takes place very frequently (IBS-D, IBS-C, IBS-M, or IBS-U respectively). IBS adversely impacts lifestyle and may result in missed out on school or work. Disorders such as stress and anxiety, major anxiety, and chronic fatigue syndrome are common amongst individuals with IBS.
This condition involves changes in frequency or type of bowel movements and lower abdominal pain.
Diet, stress, poor sleep and changes in gut bacteria may all set off symptoms.
However, triggers are various for each person, making it challenging to call particular foods or stressors that everyone with the disorder should prevent.
Symptoms of Irritable Bowel Syndrome: How You Can Tell if You Have IBS?
Let’s talk about the most common symptoms of IBS and what to do if you suspect you have it.
Symptoms of irritable bowel syndrome usually include:
Pain and Cramping
Abdominal pain is the most common symptom and an essential consider diagnosis.
Typically, your gut and brain interact to manage food digestion. This takes place via hormonal agents, nerves and signals released by the good bacteria that live in your gut.
In IBS, these cooperative signals become distorted, resulting in uncoordinated and painful tension in the muscles of the digestive tract.
This pain usually happens in the lower abdominal area or the whole abdominal area however is less most likely to be in the upper abdominal area alone. Pain usually reduces following a defecation.
Diet modifications, such as a diet low in FODMAPs, may enhance pain and other symptoms.
Other treatments consist of bowel relaxants like peppermint oil, cognitive behavior therapy and hypnotherapy.
For pain that does not respond to these changes, a gastroenterologist can help you discover a medication specifically proven to alleviate IBS pain.
The most typical symptom of IBS is lower abdominal pain that is less serious after a bowel movement. Dietary modifications, stress-reducing therapies and certain medications can help reduce pain.
Diarrhea
Diarrhea-predominant IBS is one of the three main kinds of the disorder. It impacts roughly one-third of patients with IBS.
A study of 200 adults found that those with diarrhea-predominant IBS had, usually, 12 defecation weekly – more than two times the quantity of adults without IBS.
Accelerated bowel transit in IBS can likewise result in an abrupt, immediate desire to have a bowel movement. Some patients describe this as a considerable source of stress, even avoiding some social circumstances for worry of a sudden onset of diarrhea.
Furthermore, stool in the diarrhea-predominant type tends to be loose and watery and may consist of mucus.
Frequent, loose stools prevail in IBS, and are a sign of the diarrhea-predominant type. Stools might also include mucus.
Constipation
Although it appears counterintuitive, IBS can cause constipation as well as diarrhea.
Constipation-predominant IBS is the most common type, affecting almost 50% of individuals with IBS.
Transformed communication between the brain and bowel may speed up or slow down the normal transit time of stool. When transit time slows, the bowel absorbs more water from stool, and it ends up being more difficult to pass.
Irregularity is defined as having less than three bowel movements weekly.
” Functional” irregularity explains chronic constipation not explained by another disease. It is not related to IBS and is very typical. Functional irregularity differs from IBS because it is typically not unpleasant.
On the other hand, constipation in IBS consists of abdominal pain that eases with defecation.
Constipation in IBS likewise typically triggers a sensation of an incomplete defecation. This results in unnecessary straining.
In addition to the typical treatments for IBS, workout, drinking more water, eating soluble fiber, taking probiotics and the restricted use of laxatives may assist.
Irregularity is very common. Nevertheless, abdominal pain that improves after a bowel movement and an experience of insufficient defecation after passing stool are signs of IBS.
Rotating Constipation and Diarrhea
Combined or rotating constipation and diarrhea affects about 20% of patients with IBS.
Diarrhea and constipation in IBS include chronic, repeating abdominal pain. Pain is the most essential hint that changes in defecation are not connected to diet or common, mild infections.
This type of IBS tends to be more severe than the others with more regular and intense symptoms.
The symptoms of combined IBS likewise differ more from someone to another. For that reason, this condition requires a customized treatment method rather than “one-size-fits-all” recommendations.
About 20% of patients with IBS experience alternating durations of diarrhea and irregularity. Throughout each phase, they continue to experience pain alleviated by bowel movements.
Changes in Bowel Movements
Slow-moving stool in the intestinal tract often ends up being dehydrated as the intestinal tract soaks up water. In turn, this creates hard stool, which can worsen symptoms of constipation.
Trigger motion of stool through the intestine leaves little time for absorption of water and results in the loose stools characteristic of diarrhea.
IBS can likewise cause mucus to build up in stool, which is not usually related to other causes of irregularity.
Blood in stool might signify another, potentially major medical condition and deserves a visit to your doctor. Blood in stool may appear red however often appears very dark or black with a tarry consistency.
IBS changes the time stool stays in your intestinal tracts. This changes the quantity of water in stool, providing it a range from loose and watery to hard and dry.
Gas and Bloating
Transformed food digestion in IBS causes more gas production in the gut. This can trigger bloating, which is uneasy.
Lots of with IBS identify bloating as one of the most consistent and nagging symptoms of the disorder.
In a research study of 337 IBS patients, 83% reported bloating and constraining. Both symptoms were more common in women and in constipation-predominant IBS or mixed kinds of IBS.
Preventing lactose and other FODMAPs can help reduce bloating.
Gas and bloating are some of the most typical and discouraging symptoms of IBS. Following a low-FODMAPs diet can help in reducing bloating.
Food Intolerance
As much as 70% of individuals with IBS report that specific foods trigger symptoms.
Two-thirds of people with IBS actively avoid particular foods. Sometimes these people leave out multiple foods from the diet.
Why these foods set off symptoms is uncertain. These food intolerances are not allergic reactions, and set off foods don’t trigger measurable differences in food digestion.
While trigger foods are different for everyone, some typical ones consist of gas-producing foods, such as FODMAPs, along with lactose and gluten.
Lots of people with IBS report specific trigger foods. Some common triggers consist of FODMAPs and stimulants, such as caffeine.
Fatigue and Difficulty Sleeping
Over half of people with IBS report tiredness.
In one research study, 160 adults detected with IBS explained low endurance that limited physical exertion in work, leisure and social interactions.
Another research study of 85 adults found that the intensity of their symptoms anticipated the severity of fatigue.
IBS is also related to insomnia, that includes difficulty dropping off to sleep, waking often and feeling unrested in the early morning.
In a study of 112 adults with IBS, 13% reported poor sleep quality.
Another research study of 50 men and women found that those with IBS slept about an hour longer yet felt less refreshed in the early morning than those without IBS.
Surprisingly, bad sleep anticipates more serious gastrointestinal symptoms the following day.
Those with IBS are more tired and report less refreshing sleep compared to those without it. Fatigue and poor sleep quality are also related to more extreme gastrointestinal symptoms.
Anxiety and Depression
IBS is connected to stress and anxiety and depression, too.
It’s unclear whether IBS symptoms are an expression of psychological stress or whether the stress of living with IBS makes people more prone to mental troubles.
Whichever comes first, anxiety and digestion IBS symptoms strengthen one another in a vicious cycle.
In a large research study of 94,000 men and women, people with IBS were over 50% more likely to have a stress and anxiety condition and over 70% more likely to have a state of mind condition, such as anxiety.
Another research study compared levels of the stress hormone cortisol in patients with and without IBS. Given a public speaking task, those with IBS experienced higher changes in cortisol, suggesting higher stress levels.
Additionally, another research study found that anxiety decrease therapy reduced stress and IBS symptoms.
IBS can produce a vicious circle of digestion symptoms that increase stress and anxiety and anxiety that increases gastrointestinal symptoms. Dealing with stress and anxiety can help in reducing other symptoms.
Secondary Signs of IBS
IBS can also trigger:
- farting (flatulence).
- passing mucus from your bottom.
- fatigue and an absence of energy.
- feeling ill (queasiness).
- backache.
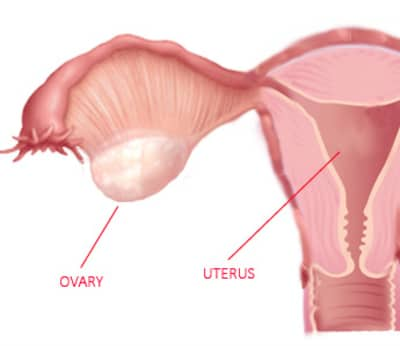
- problems peeing — like requiring to pee often, abrupt advises to pee, and feeling like you can not fully empty your bladder.
- not constantly having the ability to control when you poo (incontinence).
What to Do If You Think You Have IBS
If you have symptoms of IBS that disrupt your quality of life, visit your doctor, who can help detect IBS and eliminate other diseases that simulate it.
IBS is detected by persistent abdominal pain for a minimum of 6 months, integrated with weekly pain for 3 months along with some mix of pain alleviated by bowel movements and changes in frequency or form of defecation.
Your doctor might refer you to a gastroenterologist, a specialist in digestive diseases, who can assist you recognize triggers and go over methods to control your symptoms.
Lifestyle changes, such as a low-FODMAPs diet, stress relief, exercise, drinking a lot of water and over the counter laxatives can likewise assist. Surprisingly, a low-FODMAPs diet is one of the most promising lifestyle changes for relieving symptoms.
Determining other trigger foods can be hard, as these are various for each person. Keeping a diary of meals and active ingredients can help recognize triggers.
Probiotic supplements may also reduce symptoms.
Furthermore, avoiding gastrointestinal stimulants, such as caffeine, alcohol and sugary beverages, can lower symptoms in some individuals.
If your symptoms don’t respond to way of life changes or over the counter treatments, there are several medications shown to help in hard cases.
If you think you have IBS, think about keeping a journal of foods and symptoms. Then, take this information to your doctor to assist detect and control the condition.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.