Diabetic neuropathy is a kind of nerve damage that can take place if you have diabetes. High blood sugar level (glucose) can hurt nerves throughout your body. Diabetic neuropathy frequently damages nerves in your legs and feet.
Depending upon the affected nerves, symptoms of diabetic neuropathy can range from pain and numbness in your legs and feet to problems with your digestive system, urinary tract, blood vessels and heart. Some people have mild symptoms. However for others, diabetic neuropathy can be quite painful and disabling.
Diabetic neuropathy is a typical and serious problem of diabetes. But you can frequently prevent diabetic neuropathy or slow its development with tight blood sugar control and a healthy way of life.
Symptoms of Diabetic Neuropathy
There are 4 main types of diabetic neuropathy. You can have one or more than one kind of neuropathy. Your symptoms will depend upon the type you have and which nerves are impacted. Generally, symptoms develop slowly. You may not discover anything wrong till considerable nerve damage has actually occurred.
Peripheral neuropathy
Peripheral neuropathy is the most common type of diabetic neuropathy. It affects the feet and legs first, followed by the hands and arms. Symptoms and signs of peripheral neuropathy are typically even worse in the evening, and might include:
- Numbness or lowered ability to feel pain or temperature changes
- Tingling or burning experience
- Acute pains or cramps
- Increased sensitivity to touch– for some people, even the weight of a bedsheet can be painful
- Muscle weakness
- Loss of reflexes, particularly in the ankle
- Vertigo and coordination
- Serious foot problems, such as ulcers, infections, and bone and joint pain
- Autonomic neuropathy
The free anxious system controls your heart, bladder, stomach, intestines, sex organs and eyes. Diabetes can impact nerves in any of these areas, perhaps triggering:
- A lack of awareness that blood sugar level levels are low (hypoglycemia unawareness).
- Bladder issues, consisting of urinary tract infections or urinary retention or incontinence.
- Constipation, unchecked diarrhea or both.
- Sluggish stomach emptying (gastroparesis), causing queasiness, vomiting, bloating and anorexia nervosa.
- Difficulty swallowing.
- Increased or reduced sweating.
- Issues managing body temperature.
- Changes in the method your eyes adjust from light to dark.
- Increased heart rate at rest.
- Sharp drops in high blood pressure after sitting or standing that might cause you to faint or feel lightheaded.
- Impotence.
- Vaginal dryness.
- Reduced sexual action.
- Radiculoplexus neuropathy (diabetic amyotrophy).
Radiculoplexus neuropathy affects nerves in the thighs, hips, buttocks or legs. It’s more common in individuals with type 2 diabetes and older adults. Other names for this type are diabetic amyotrophy, femoral neuropathy or proximal neuropathy.
Symptoms are usually on one side of the body, but sometimes may spread to the opposite. You might have:
- Extreme pain in a hip and thigh or butt that happens in a day or more.
- Ultimate weak and diminishing thigh muscles.
- Difficulty increasing from a sitting position.
- Stomach swelling, if the abdominal area is impacted.
- Weight-loss.
Many people enhance a minimum of partially in time, though symptoms might aggravate prior to they get much better.
Mononeuropathy
Mononeuropathy, or focal neuropathy, is damage to a particular nerve in the face, middle of the body (upper body) or leg. It’s most common in older adults. Mononeuropathy typically strikes unexpectedly and can cause extreme pain. Nevertheless, it usually does not cause any long-lasting problems.
Symptoms usually disappear without treatment over a few weeks or months. Your particular signs and symptoms depend upon which nerve is included. You may have pain in the:
- Shin or foot.
- Lower back or pelvis.
- Front of thigh.
- Chest or abdomen.
Mononeuropathy might likewise trigger nerve issues in the eyes and face, leading to:
- Trouble focusing.
- Double vision.
- Aching behind one eye.
- Paralysis on one side of your face (Bell’s palsy).
In some cases mononeuropathy happens when something is continuing a nerve (nerve compression). Carpal tunnel syndrome is a typical type of compression neuropathy in people with diabetes. It can cause numbness or tingling in your hand or fingers, except your pinkie (little finger). Your hand may feel weak, and you may drop things.
When to see a doctor
Call your doctor for a visit if you have:
- A cut or sore on your foot that is infected or will not recover.
- Burning, tingling, weakness or pain in your hands or feet that interferes with everyday activities or sleep.
- Changes in food digestion, urination or sexual function.
- Dizziness.
These symptoms and signs don’t always indicate you have nerve damage. But they can be an indication of another condition that needs treatment. Early diagnosis and treatment of any health condition gives you the very best chance for controlling your diabetes and preventing future problems.
Causes of Diabetic Neuropathy (Nerve Pain)
Damage to nerves and blood vessels
The exact cause likely differs for each type of neuropathy. Researchers believe that with time, unchecked high blood sugar damages nerves and hinders their capability to send signals, causing diabetic neuropathy. High blood glucose also weakens the walls of the little capillary (capillaries) that supply the nerves with oxygen and nutrients.
However, a combination of factors might result in nerve damage, consisting of:
- Inflammation in the nerves brought on by an autoimmune response. The immune system mistakes nerves as foreign and attacks them.
- Hereditary factors unassociated to diabetes might make some individuals most likely to establish nerve damage.
- Smoking and alcohol abuse damage both nerves and blood vessels and significantly increase the threat of infection.
Risk Factors
Anyone who has diabetes can develop neuropathy, however these danger factors make you most likely to get nerve damage:
- Poor blood sugar control. Unchecked blood glucose puts you at risk of every diabetes problem, including nerve damage.
- Diabetes history. Your danger of diabetic neuropathy increases the longer you have diabetes, particularly if your blood sugar level isn’t well-controlled.
- Kidney disease. Diabetes can damage the kidneys. Kidney damage sends out toxic substances into the blood, which can cause nerve damage.
- Being overweight. Having a body mass index (BMI) higher than 24 may increase your danger of diabetic neuropathy.
- Smoking cigarettes. Smoking cigarettes narrows and solidifies your arteries, lowering blood circulation to your legs and feet. This makes it more difficult for injuries to heal and harms the peripheral nerves.
Complications
Diabetic neuropathy can cause a variety of serious problems, consisting of:
- Loss of a toe, foot or leg. Nerve damage can make you lose feeling in your feet. Foot sores and cuts might silently end up being seriously infected or become ulcers. Even small foot sores that do not heal can turn into ulcers. In serious cases, infection can spread out to the bone, and ulcers can lead to tissue death (gangrene). Removal (amputation) of a toe, foot or even the lower leg might be needed.
- Joint damage. Nerve damage can trigger a joint to degrade, causing a condition called Charcot joint. This usually takes place in the small joints in the feet. Symptoms include loss of feeling and joint swelling, instability and in some cases joint defect. Trigger treatment can assist you heal and prevent further joint damage.
- Urinary tract infections and urinary incontinence. If the nerves that manage your bladder are harmed, you may be not able to fully clear your bladder. Bacteria can develop in the bladder and kidneys, causing urinary tract infections. Nerve damage can likewise affect your capability to feel when you require to urinate or to control the muscles that launch urine, causing leak (incontinence).
- Hypoglycemia unawareness. Low blood sugar level (below 70 milligrams per deciliter, or mg/dL) usually causes shakiness, sweating and a fast heartbeat. But if you have autonomic neuropathy, you might not notice these caution signs.
- Sharp drops in blood pressure. Damage to the nerves that manage blood flow can impact your body’s ability to change high blood pressure. This can trigger a sharp drop in pressure when you stand after sitting (orthostatic hypotension), which may result in lightheadedness and fainting.
- Gastrointestinal problems. If nerve damage strikes your digestion tract, you can have constipation or diarrhea, or bouts of both. Diabetes-related nerve damage can lead to gastroparesis, a condition in which the stomach clears too gradually or not at all. This can interfere with digestion and significantly impact blood glucose levels and nutrition. Symptoms and signs include queasiness, vomiting and bloating.
- Sexual dysfunction. Autonomic neuropathy often damages the nerves that impact the sex organs. Men may experience erectile dysfunction. Women might have difficulty with lubrication and arousal.
- Increased or reduced sweating. Nerve damage can disrupt how your sweat glands work and make it tough for your body to manage its temperature level appropriately. Some individuals with autonomic neuropathy have excessive sweating, particularly during the night or while consuming. Too little or no sweating at all (anhidrosis) can be lethal.
Treatment for Diabetic Neuropathy
Nerve pain brought on by diabetes, referred to as diabetic peripheral neuropathy, can be extreme, continuous, and difficult to treat. It may begin as a tingling feeling, followed by numbness and pain. But there are two bottom lines that everybody with diabetes and peripheral neuropathy ought to know:
- Managing your blood sugar can keep the pain from getting even worse and improve your health.
- Medications can help eliminate nerve pain, make you more comfy, and improve your quality of life.
- Start With Blood Sugar
If you have diabetes and peripheral neuropathy, talk with your physician about how to handle your blood sugar levels. That may mean you require to take insulin.
Once you’re doing all you can to keep your blood sugar level in check– including diet, meal planning, workout, and medication– ask the doctor which pain treatment might best relieve the rest of your symptoms.
There are numerous medications that can alleviate nerve pain and help you work at near-normal levels. But you may require to try several different types prior to you find the one that works finest.
Over-the-Counter (OTC) Pain Relievers for Diabetic Nerve Pain
Some individuals find relief right on drugstore shelves. Common painkiller and some skin creams may help. It depends upon how severe your pain is.
Speak with your doctor before taking any product. Even over the counter medications can communicate with other drugs or trigger severe side impacts. Here are some choices:
NSAIDS for Diabetic Nerve Pain
NSAIDs (nonsteroidal anti-inflammatory drugs) minimize inflammation and relieve pain. Those readily available without a prescription consist of aspirin, ibuprofen (Advil, Motrin, Nuprin), and naproxen (Naprosyn).
But NSAIDs are known to increase the risk of heart attack and stroke, specifically when taken in high dosages. They can also trigger harmful adverse effects like stomach inflammation and bleeding if you take them for a long time. They can also result in or intensify pre-existing kidney damage, which might be more most likely in people with diabetes.
Acetaminophen and other over-the-counter drugs which contain it alleviate pain without reducing inflammation. These medications do not trigger the stomach inflammation that NSAIDs do, but taking more than suggested can result in liver damage. Read labels and talk to your pharmacist.
Capsaicin is discovered naturally in chili peppers. It’s believed to manage a chemical called compound P, which helps send out pain signals through your nerves. It can assist in the short term, however there are concerns about long-lasting use. That’s because these exact same nerves play a role in injury healing, a procedure that’s currently a problem if you have diabetes.
Lidocaine is an anesthetic that numbs the area it’s used to. It’s offered in gels and creams, both over the counter and by prescription.
Prescription Drugs for Diabetic Nerve Pain
Many individuals need to turn to prescription medication to find relief.
NSAIDs are likewise readily available by prescription. They might be various doses or different drugs entirely from what’s provided without a prescription.The side impacts – stomach problem and greater chances of heart problem – are the very same similar to other types.
Antidepressants
Antidepressants treat anxiety however have also ended up being crucial in easing chronic pain. They can work whether you’re depressed or not. Those utilized to treat pain include:
- Tricyclic antidepressants, which impact the levels of the brain chemicals norepinephrine and serotonin. Experts state they’re the most reliable of the antidepressants used for pain. But they likewise cause side results, like sleepiness, weight gain, dry mouth, and dry eyes. Blood pressure, heart rate problems, and lightheadedness can likewise occur with these drugs.
- Selective serotonin reuptake inhibitors (SSRIs), which work by modifying the amount of the brain chemical serotonin. They’re efficient for depression but less useful for pain.
- Serotonin and norepinephrine reuptake inhibitors (SNRIs), which treat anxiety by enhancing the brain chemicals serotonin and norepinephrine. They may have fewer side impacts than the SSRIs or TCAs.
Antiseizure drugs, used to prevent epileptic seizures, can likewise alleviate neuropathy. The drugs manage the nerve cells in the brain and other parts of your body, such as legs and arms, that transfer pain. But they can make you dizzy or drowsy, specifically at high doses.
Opioid medications
When your problem is serious, you desire immediate relief. That’s when you ought to see a pain expert. You may require strong medicines that consist of a weak opioid (a morphine-like substance). These drugs also impact the brain chemicals serotonin and norepinephrine, similar to antidepressants, and decrease your feeling of pain.
Opioids can provide a much better option for “advancement pain” – a kind that all of a sudden intensifies for no obvious factor – than OTC drugs.
Neuropathy professionals avoid strong narcotic opioid medications. They can trigger extreme constipation, and there’s an opportunity you might get addicted. There’s likewise a stigma linked with using this kind of drug. And depending upon the kind of work you do, it might be an issue.
More Treatment Options
Injections of anesthetics like lidocaine – or spots that contain it – can likewise numb the area.
Physicians might likewise:
- Surgically ruin nerves or alleviate a nerve compression that causes pain
- Implant a device that eliminates pain
- Carry out electrical nerve stimulation which might ease pain. In this treatment, small amounts of electricity are used to block pain signals as they travel through the skin. Experts state its effectiveness is debatable.
Other beneficial aids to improve your quality of life consist of:
- Hand or foot braces that can help muscle weakness or relieve nerve compression
- Orthopedic shoes that can improve strolling issues, which will prevent foot injuries.
Questions and Answers
Diabetic neuropathy, as a complex disease, requires answering many related questions from symptoms to treatment and medications used. Your doctor will help you answer them. In this section we have collected the most frequently asked questions from patients with diabetes nerve pain:
What is the modified Thomas classification system for diabetic neuropathy?
Two classification systems for diabetic neuropathy are the Thomas system and the symmetrical-versus-asymmetrical system. The Thomas system (modified) is as follows:
- Hyperglycemic neuropathy
- Generalized symmetrical polyneuropathies
- Sensory neuropathy
- Sensorimotor neuropathy
- Autonomic neuropathy
- Focal and multifocal neuropathies
- Superimposed chronic inflammatory demyelinating polyneuropathy
How is diabetic polyneuropathy staged?
Diabetic polyneuropathy is frequently staged as follows:
- NO – No neuropathy
- N1a – Signs but no symptoms of neuropathy
- N2a – Symptomatic mild diabetic polyneuropathy; sensory, motor, or autonomic symptoms; patient has the ability to heel-walk
- N2b – Severe symptomatic diabetic polyneuropathy; client is not able to heel-walk).
- N3 – Disabling diabetic polyneuropathy.
What are the essential elements of diabetic neuropathy management?
Secret parts of the management of diabetic neuropathy include the following:.
- Foot care, consisting of regular follow-up, client education, and recommendation as suitable.
- Tight, stable glycemic control (crucial for slowing progression of neuropathy).
- Pain management (eg, with pregabalin, gabapentin, sodium valproate, dextromethorphan, morphine sulfate, tramadol, oxycodone, duloxetine, topical capsaicin, transdermal lidocaine).
- Treatment of diabetic gastroparesis (eg, with erythromycin, cisapride [not available in the United States], metoclopramide, polyethylene glycol 3350, tegaserod [currently offered only on an emergency basis].
- Speculative therapies include aldose reductase inhibitors, alpha-lipoic acid, actovegin, and back cord stimulators.
What are the surgical options for diabetic neuropathy?
Surgical treatment might be thought about as follows:
- Aggressive debridement or amputation for recalcitrant foot necrosis or infection.
- Jejunostomy for intractable gastroparesis.
- Implantation of a penile prosthesis for continuous impotence.
- Bracing, unique boots, or, sometimes, surgery for Charcot foot.
- Pancreatic transplantation for diabetes with end-stage renal disease.
What is the frequency of diabetic neuropathy?
Neuropathies are the most common issue of diabetes mellitus (DM), impacting approximately 50% of patients with type 1 and type 2 DM. In type 1 diabetes mellitus, distal polyneuropathy typically becomes symptomatic after several years of chronic extended hyperglycemia. Alternatively, patients with type 2 diabetes mellitus may provide with distal polyneuropathy after just a few years of known bad glycemic control; sometimes, these patients currently have neuropathy at the time of diagnosis.
What are secondary complications of diabetic neuropathy?
Neuropathies severely reduce patients’ quality of life (QOL). In addition, while the primary symptoms of neuropathy can be extremely unpleasant, the secondary problems (eg, falls, foot ulcers, cardiac arrhythmias, and ileus) are even more major and can result in fractures, amputations, and even death in patients with DM.
What are the manifestations of diabetic neuropathy?
Since diabetic neuropathy can manifest with a wide array of sensory, motor, and free symptoms, a structured list of symptoms can be utilized to help screen all diabetic patients for possible neuropathy. Physical examination of patients with thought distal sensory motor or focal (ie, entrapment or noncompressive) neuropathies need to include evaluations for both peripheral and free neuropathy.
What are the danger elements connected with extreme symptoms of diabetic neuropathy?
Danger factors that are related to more serious symptoms include the following:
- Poor glycemic control.
- Advanced age.
- High blood pressure.
- Long period of time of DM.
- Dyslipidemia.
- Smoking.
- Alcohol intake.
- HLA-DR3/ 4 phenotype.
- Tall height.
How do symptoms of diabetic neuropathy develop?
Development of symptoms depends upon many factors, such as total hyperglycemic direct exposure and other risk elements such as elevated lipids, blood pressure, smoking, increased height, and high exposure to other possibly neurotoxic agents such as ethanol. Hereditary elements may also play a role.
What is the death rate for diabetic neuropathy?
Mortality is higher in people with cardiovascular free neuropathy (CAN). The total mortality rate over periods approximately 10 years was 27% in patients with DM and CAN discovered, compared to a 5% mortality rate in those without proof of CAN. Morbidity results from foot ulceration and lower-extremity amputation. These 2 complications are the most common causes of hospitalization among individuals with DM in Western countries. Serious pain, dizziness, diarrhea, and impotence are typical symptoms that reduce the QOL of a patient with DM. In patients with diabetic peripheral neuropathy, the prognosis is good, however the patient’s QOL is decreased.
How does tertiary care impact the results of diabetic neuropathy?
In a Canadian research study of patients with painful diabetic neuropathy being handled in a tertiary care setting, Mai et al found that at 12-month follow-up, considerable enhancement in pain and function had been accomplished in nearly one third of these people. That included pain decrease of 30% or higher in 37.2% of patients, functional enhancement (decrease of 1 or higher on the Pain Interference Scale) in 51.2% of patients, and achievement of both of these measures in 30.2% of patients. Polypharmacy was discovered to be necessary to sign management and consisted of the use of analgesic antidepressants and anticonvulsants.
What is the role of diet and nutrition in the management of diabetic neuropathy?
Controlling diet and nutrition are vital to improving the secondary issues of diabetes, including neuropathy. Patients with diabetic neuropathy should deal with nutritionists or their medical care doctors to establish a sensible diet for reducing blood glucose and lessening large fluctuations in blood sugar.
What activity modifications are required for patients with diabetic neuropathy?
Patients with diabetic neuropathy need to be encouraged to stay as active as possible. However, those with substantial sensory loss or autonomic dysfunction need to be warned about working out in extreme climate condition, which might lead to injury. For example, patients with extremity numbness might not know frostbite injuries during extended cold direct exposure, or those with abnormal sweating might end up being quickly overheated in hot conditions. Most of the times, assessment with the patient’s regular physician is reasonable prior to the initiation of a routine exercise program.
What foot defense and care guidelines should patients with diabetic neuropathy get?
The value of security and care of insensitive feet can not be overemphasized. Patients must be instructed to trim their toenails with great care and to be fastidious about foot health. Any fungal or bacterial infection requireds prompt medical attention. The need for well-fitting shoes should be stressed.
What are the ophthalmologic and renal conditions connected with diabetic neuropathy?
Diabetic polyneuropathy is typically related to diabetic retinopathy and nephropathy. Patients with neuropathy ought to be counseled to look for proper eye care and go over renal care and follow-up with their main care physicians or endocrinologists.
Which medications are utilized in the treatment of diabetic neuropathic pain?
Many medications are offered for the treatment of diabetic neuropathic pain. Oral agents consist of antidepressants and anticonvulsant drugs. According to the 2011 guideline issued by the American Academy of Neurology (AAN), American Academy of Physical Medicine and Rehabilitation (AANEM) and the American Academy of Physical Medicine and Rehabilitation (AAPMR) guideline for the treatment of painful diabetic neuropathy (PDN), pregabalin is suggested for treatment of diabetic neuropathic pain. The drug has been proven reliable and can improve quality of life. Nevertheless, doctors ought to figure out if the drug is clinically suitable for their patients on a case-by-case basis. Gabapentin and sodium valproate should also be considered for diabetic neuropathy pain management.
What is the function of gabapentin in the treatment of diabetic neuropathy?
According to a Cochrane evaluation examining gabapentin for chronic neuropathic pain and fibromyalgia, gabapentin causes substantial pain relief in patients with chronic neuropathic pain when compared with a placebo. Although patients often experience adverse side effects, these are typically bearable, and severe adverse effects were not increased when compared with negative effects connected with the placebo.
Which medications are utilized to control diabetic neuropathic pain throughout pregnancy?
During pregnancy, prescribing medicine for pain control is challenging. The very best expect pain control in unusual cases of girls with serious neuropathy is to control their blood sugar diligently and attempt to control pain with acetaminophen. At the end of the 3rd trimester, the physician can prescribe amitriptyline, gabapentin, and other medications as shown if the benefit plainly surpasses the threat to the fetus. Physical treatment may be efficient in pregnant patients by increasing their flow.
What is the role of dietary supplements in the treatment of diabetic neuropathy?
Vitamin supplementation is being studied to see if that can have an effect. One research study of zinc sulfide showed enhancement in glycemic control in 60 patients. Certain B vitamins are frequently recommended in an attempt to reduce paresthesias.
What is the function of spine stimulator implants in the treatment of diabetic neuropathy?
Pain medication experts have actually been try out spine stimulator implants in badly painful cases. One such research study of 10 patients showed that median background and peak pain ratings at the end of the research study were, respectively, 77 and 81 with the stimulator off and 23 and 20 with the stimulator on. Workout tolerance substantially enhanced at 3 months (n = 7, median increase 85%) and at 6 months. Additional study is necessary.
How is erectile dysfunction due to diabetic neuropathy treated?
Although numerous techniques are offered, erectile dysfunction from diabetic neuropathy is a very difficult condition to deal with. All other causes of impotence must be excluded. As soon as the diagnosis has actually been validated, the oral agent sildenafil Viagra) and associated phosphodiesterase type 5 (PDE5) inhibitors can be used (if not contraindicated in the client). Older techniques such as vacuum gadgets or intracavernosal papaverine injections may be tried. Referral to a urologist is suggested.
How are feet issues of diabetic neuropathy treated?
The feet of patients with DM frequently end up being insensate and are extremely vulnerable not just to ulcers however likewise to the Charcot foot (ie, a foot that loses its structure secondary to injury and acute arthropathy) from frequent and multiple traumas. Charcot foot, which takes place not just in diabetic peripheral neuropathy but in other types of serious neuropathy also, can be treated with bracing or unique boots. In some cases, surgery is used to fix the defect.
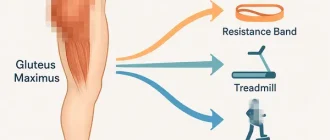
What is the role of physical therapy in the treatment of diabetic neuropathy?
Physical therapy may be an useful adjunct to other treatment, especially when muscular pain and weakness are a manifestation of the client’s neuropathy. The physical therapist can instruct the patient in a general exercise program to maintain his/her mobility and strength. An aquatic therapist can likewise be handy.
Although the American Diabetes Association recommends moderate to energetic workout for patients with diabetes to assist handle the disease, a literature evaluation by Johnson and Takemoto showed that in patients who have actually been inactive or can not accomplish such intensity levels, low-intensity aerobic therapy can enhance sensation in the feet and minimize pain and tingling in the lower limbs.
What is the role of transcutaneous electrical nerve stimulation (TENS) in the treatment of diabetic neuropathy?
In addition to workout, the client likewise should be informed on independent pain management and relaxation methods to assist with pain control. Transcutaneous electrical nerve stimulation (TENS) might be a recommended technique for patients with neuropathic pain, and the physical therapist can be handy in teaching and keeping an eye on the client in its use. In a 1999 case report, Somers and Somers discovered that application of TENS to the skin of the back area was an effective treatment for the pain of diabetic neuropathy, but no regulated research studies have actually confirmed this finding. The 2011 AAN/AANEM/AAPMR guideline supports TENS as most likely reliable as a treatment for PDN.
Used sources: www.webmd.com, www.mayoclinic.org, emedicine.medscape.com
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.