Allergic rhinitis – inflammation of the nasal mucosa – can rightfully be attributed to a disease with which 100% of the world’s population is familiar. Regardless of the causes of the disease and how severe it is, everyone faces a runny nose.
But the prevalence of this disease does not make it less threatening – if untreated, it can become the onset of more serious medical problems (sinusitis, mucosal atrophy) and make a person vulnerable to dangerous infections.
Allergic Rhinitis Causes
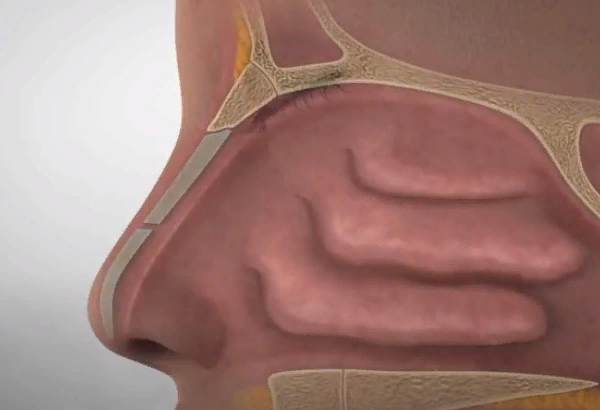
Allergic rhinitis (AR) is a chronic inflammatory disease of the nasal mucosa caused by exposure to a causal allergen. It is manifested by itching, sneezing, rhinorrhea (profuse nasal discharge), nasal congestion and sometimes conjunctivitis. Symptoms most often come on contact with plant pollen, dust, animal hair, or other allergens.
In most cases, the causes of the common cold are viral infections that affect the mucous membrane of the nasal cavity and cause its inflammation. If the treatment is not carried out on time, bacterial ones join the primary infection, making the course of the disease more severe, and provoking the development of a number of complications.
But with a prolonged, persistent runny nose or nasal congestion, the following factors can be the causes of these conditions:
- Diseases of the organs of the oropharynx and nasopharynx. In this case, the course of the rhinitis is supported by infections present on the palatine tonsils, in the maxillary sinuses and even in the oral cavity.
- Hypersensitivity of the immune system. Allergic rhinitis in adults and children develops in response to contact of the mucous membrane of the conjunctiva and nasal cavity with any substance that the immune system perceives as foreign.
- Dysfunction of the mucous membrane of the nasal cavity. The long course of rhinitis, whatever the cause, gradually leads to mucosal atrophy (thinning and loss of the ability to produce mucus), mucosal hypertrophy (its abnormal thickening, up to complete blockage of the nasal passages) and disruption of the neurovascular system of the mucosa.
- Mucosal injury. This list includes a wide range of circumstances – from careless cleansing of the nose and direct trauma to the mucous membrane, to foreign bodies in the nasal cavity, disrupting the blood circulation of tissues and becoming a focus of infection
But the question remains: why some people are more prone to rhinitis and suffer from it regularly, while others – relatively rarely encounter a runny nose. The reason for this uneven “distribution” is predisposing factors.
Predisposing Factors
The circumstances that increase the likelihood of developing rhinitis and other acute respiratory viral infections are:
- violation of the body’s defenses caused by a chronic or acute course of diseases of the digestive system, vascular disorders, etc.;
- inappropriate nutrition with a deficiency in the diet of nutrients and biologically active substances;
- professional or daily employment, involving contact with volatile chemicals (for example, with paints and varnishes) and staying in a gas-polluted, dusty room without personal protective equipment;
- hereditary predisposition to respiratory allergies (in the family history there are / were cases when any of the relatives suffered from allergic rhinitis or conjunctivitis);
- smoking and alcohol;
- frequent and / or inappropriate use of vasoconstrictor drops or nasal sprays.
How allergic rhinitis occurs
A type 1 immunopathological reaction, manifested by the formation and fixation of specific class E immunoglobulins (IgE) on mast cells and basophils, develops when the body is exposed to a causative allergen. Repeated encounter with the allergen leads to immunoglobulin E-dependent activation of mast cells in the airway mucosa, which causes the release of inflammatory mediators from mast cell granules and basophils. These mediators cause vasodilation, swelling and thickening of the airway mucosa, and increase mucus secretion.
The first phase is the immediate, acute response to the allergen. This phase develops within minutes of exposure to the allergen. The allergen binds with specific IgE fixed on mast cells, which leads to activation of these cells and release of inflammatory mediators (such as histamine, tryptase, chymase, platelet-activating factor, etc.). Inflammatory mediators affect neuroreceptors and as a result there is an increase in vascular permeability, mucus hypersecretion, contraction of smooth muscles, occurrence of acute symptoms of allergic diseases: sneezing, nasal mucosa swelling and nasal itching.
In 70% of patients suffering from allergic diseases the second phase – late, delayed response – begins 6 to 12 hours after exposure to the allergen. The immune system cells (CD4+, Th2-lymphocytes, eosinophils, basophils, neutrophils) tighten up to the place of allergic inflammation, at the same time cytokines and leukotriens, the mediators of inflammation, are released into blood. As a result, chronic allergic mucosal inflammation and airway hyperresponsiveness are formed.
Classification and developmental stages of allergic rhinitis
The Allergic Rhinitis and Its Impact on Asthma (ARIA) working group guidelines propose a classification of allergic rhinitis based on an assessment of the impact of allergic rhinitis on patients’ quality of life:
- Intermittent allergic rhinitis – symptoms bother the patient less than 4 days per week or less than 4 weeks per year;
- persistent allergic rhinitis – symptoms bother the patient more than 4 days per week or more than 4 weeks per year.
By severity:
Mild stage. Symptoms are minimally expressed, do not bother the patient significantly: sleep and daytime activity do not suffer, school work does not decrease.
The average severity/severe stage. Symptoms significantly disturb the patient: impaired sleep, daytime activity and performance, reduced school performance.
Also distinguished:
Seasonal allergic rhinitis – complaints appear within a few hours after contact with an allergen, such as pollen from flowering plants. 30-40% of children with pollinosis (pollen allergy) develop bronchial asthma, most often in the spring, summer or early fall.
Year-round allergic rhinitis – symptoms occur more than 2 hours a day and for at least 9 months a year, usually occurs with sensitization (hypersensitivity) to household allergens (house dust mites, cockroaches, molds).
However, this classification of allergic rhinitis has weaknesses. For example, some countries have pollen all year round (Mediterranean countries, India, etc.). Allergies to mites can also give peaks of exacerbations not year-round, but only in the season of their maximum reproduction – autumn-spring.
Allergic rhinitis has two stages:
- acute exacerbation;
- remission.
Almost all patients with a mild course of allergic rhinitis believe that it is possible to live with it without prescription of medicines and monitoring by a doctor.
Complications of allergic rhinitis
Allergic rhinitis that is not detected in time is often complicated. Possible complications include:
- Secretory otitis media – inflammation of the middle ear, accompanied by the accumulation of exudate (inflammatory fluid) in the middle ear cavities and decreased hearing;
- hypertrophy (enlargement) of the tonsils;
- Chronic sinusitis – inflammation of the sinuses;
- nasal polyposis.
Allergic rhinitis is not considered a life-threatening condition, but it can severely impair quality of life. Due to the absence of normal nasal breathing, patients often feel irritable, tired, worn out, their grades and performance plummet. 90% of children with allergic rhinitis have a sleep disorder.
Allergic rhinitis can lead to permanent swelling and an increase in the size of the nasal cavities and tonsils (hypertrophy). This causes persistent, uncontrollable nasal congestion, headache, frequent infections of the sinuses and middle ear, sleep apnea, development of dental bite anomalies (constant breathing through the mouth leads to deformities of the facial skeleton). This problem may require surgical treatment.
It is also necessary to remember the relationship between allergic rhinitis and bronchial asthma. Studies show that allergic rhinitis patients develop inflammation in the bronchi when exposed to a causative allergen. Inflammation can be maintained and exacerbated by interrelated mechanisms, meaning that if allergic rhinitis is not controlled, there is a high risk of developing or exacerbating bronchial asthma and other allergic diseases.
Allergic Rhinitis Treatment
In the treatment of acute and chronic rhinitis of any origin, the principles of treatment are generally similar, and the goals of therapy are the following areas:
- Restoration of nasal breathing. For this, a wide range of drugs is used, the action of which is aimed at eliminating edema of the nasal mucosa and normalizing mucus production.
- Restoring the patency of the airways. In this case, surgical methods can be used that make it possible to correct a deviated nasal septum, enlarged turbinates and remove hypertrophied tissues in the nasal passages (polyps).
- Elimination of the causes of infectious rhinitis. In addition to the obvious reasons – viruses and bacteria entering the nasal cavity with inhaled air – chronic or allergic rhinitis can be caused or supported by other diseases. These include almost all infectious diseases of the oral cavity, oropharynx and nasopharynx, since the direct communication of the nasal cavity with adjacent structures allows pathogens to migrate along the mucous membrane with saliva and nasal secretions.
- Relief of symptoms. Symptoms of allergic rhinitis accompanying a runny nose – headache, appetite and sleep disorders, fever, etc., although they do not pose a direct threat to health, deplete the body’s resources and significantly slow down recovery.
Treatment in most cases is performed in outpatient settings. Hospitalization is required mainly in case of disease complications.
Treatment of patients suffering from allergic rhinitis should be prescribed taking into account the individual characteristics of the body. It will include:
- Elimination (elimination) of the causative allergen.
- Education (allergy schools). The format of the training can be different: it can be websites containing lectures and advice, as well as live broadcasts and offline meetings of the doctor with those wishing to attend. The training cycle includes a discussion of the main issues of the problem: the causes of the disease, its prevalence, manifestations, the possibility of diagnosis and treatment, and prognosis.
- Elimination of symptoms of allergic rhinitis (pharmacotherapy).
- Allergen-specific immunotherapy (ASIT).
Pharmacotherapy/Medications
- Antihistamines of systemic and local action. Aimed at inhibiting the action of free histamine. The choice between oral (by mouth) and intranasal (through the nose) antihistamines (azelastine, levocabastine) depends on patient preference, availability and price of drugs. These drugs effectively and quickly reduce nasal secretions, nasal congestion and nasal itching.
1st generation antihistamines are not recommended due to sedative effects, negative effects on cognitive function, asthma, and other comorbidities. Examples of 1st generation sedative antihistamines are: “Dimedrol”, “Tavegil”, “Pipolfen”, “Primalin”, “Suprastin”, “Fenistil”, “Atarax”, “Peritol”, “Fencarol”, “Bicarphen”.
Basic therapy for allergic rhinitis are second-generation antihistamines: Claritin, Zyrtec, Telfast, Kestin, Semprex, Allergodil, Opatanol, Erius, Xizal, Rupafin, loratadine, desloratadine, cetirizine, levocetirizine, fexofenadine.
- Mast cell membrane stabilizers of systemic and local action. These are drugs that inhibit the release of inflammatory mediators from mast cells – histamine, etc. Such drugs include cromones (sodium cromoglycate and sodium nedocromil). These are topical intranasal forms, they are safe, but have a less pronounced and long-lasting effect. They are most commonly used to treat allergic conjunctivitis and mild forms of allergic rhinitis.
- Decongestants. Intranasal vasoconstrictors, used to relieve mucosal swelling (osmometazoline, xylometazoline). Used only to relieve symptoms of nasal congestion, used for a short course (no more than 3-7 days). Decongestants do not stop allergic inflammation, so if you stop taking them, your complaints may return.
- local anticholinergic agents. Intranasal agents are especially effective in patients with pronounced rhinorrhea. Ipratropium bromide has anticholinergic effect, i.e. it reduces secretion of nasal mucous membrane glands. In therapeutic concentrations it does not irritate nasal mucosa. The action of the drug starts after 5-10 minutes and lasts for 6-8 hours.
- Glucocorticosteroids. These drugs effectively and safely eliminate the severity of such symptoms as itching, rhinorrhea and nasal congestion. Their action is aimed at suppressing inflammation, reducing the permeability of the mucosa. Regular and prolonged use is recommended to control the disease. Modern intranasal steroids, such as mometasone furoate and fluticasone furoate, are preferred in therapy. The following drugs are currently on the market:
| Active ingredient | Systemic bioavailability index | Age restrictions for use |
|---|---|---|
| Mometasone furoate | Less than 0.1% | 2 yo |
| Fluticasone furoate | Less than 0,5% | 2 yo |
| Fluticasone propionate | 2,00% | 4 yo |
| Budesonide | 34,00% | 6 yo |
| Beclomethasone | 44,00% | 6 yo |
- Antileukotriene drugs (leukotriene receptor antagonists – Montelukast) reduce inflammatory processes that have an infectious or allergic cause. These are promising drugs, especially indicated in the combination of allergic rhinitis with a bronchoobstructive component and bronchial asthma. They have a high safety and efficacy profile. It can be used from the age of two years. Used for courses of at least 1-3 months.
- Allergen-specific immunotherapy (ASIT) is the only method of personalized therapy that affects the cause of the disease. It is administered by an allergologist. The therapy involves introducing small doses of an allergen into the body, which “trains” the immune system and gets used to the allergen. This allows the patient to get rid of the allergy and decrease the risk of bronchial asthma. In the Russian Federation, drugs for ASIT are available for allergies to mites, house dust, tree and grass pollen. It is given from the age of five. The route of administration is subcutaneous or under the tongue (sublingually). The course lasts 3-5 years.
Future treatments for allergic rhinitis may involve influencing the inflammatory response – cytokines (peptide molecules that transmit signals from one cell to another, prompting it to develop inflammation or, conversely, to stop it). For example, monoclonal antibodies to cytokines and their receptors, as well as anti-inflammatory cytokines, cytokine inhibitors, etc., can be used.
Non-conventional therapies such as acupuncture, homeopathy, and others have no convincing evidence base regarding their efficacy and safety.
How to Cure Allergic Rhinitis Permanently
A separate therapeutic tactic has been developed for situations where treatment of allergic rhinitis is required. In this case, treatment is based on the following principles:
- Identification of the allergen and exclusion of patient contact with this substance.
- Reducing the hypersensitivity of the immune system.
- Prescribing antihistamines to the patient and teaching behavior in situations where an allergic reaction begins.
With hay fever (seasonal allergy to the flowering of certain plants), sensitizing therapy may be prescribed, which is aimed at “accustoming” the human immune system to the allergen and reducing the intensity of the immune response. Such treatment of allergic rhinitis in adults and, to a limited extent, in children, is carried out in the cold season, when the influence of natural allergens is excluded.
Home treatment
Treatment of allergic and chronic rhinitis at home is an auxiliary form of therapy, the purpose of which is to fully cover all aspects of the disease. So, in addition to medications prescribed by a doctor, the patient can independently carry out some procedures (unless otherwise indicated by the ENT doctor):
- steam inhalations using essential oils, herbal decoctions;
- rinsing the nasal cavity with prepared solutions;
- warm foot baths;
- plentiful warm drink.
It should be remembered that at elevated body temperature, any thermal procedures are contraindicated, and if we are talking about a child, rinsing of the nasal passages is carried out only in a treatment room.
How to cure allergic rhinitis at home?
Home treatment for allergic rhinitis includes the following points:
- Elimination of contact with allergens. So, if allergy tests have identified house dust as an allergen, then heavy textile curtains, carpets and other interior items that accumulate dust should be removed from the premises.
- With hay fever (seasonal allergic rhinitis), you should visit a doctor in advance and get an appointment. And take antihistamines with the onset of flowering of the allergen plant. In addition, outdoor exposure should be minimized in windy conditions when pollen travels long distances.
- Treatment for allergic rhinitis may also include dietary adjustments. This is due to the fact that hyperallergenic foods (citrus fruits, honey, seafood, chocolate, etc.) can cause cross-allergies and increase the course of hay fever.
Symptoms and treatment of allergic rhinitis are closely related: the more intense the reaction of the immune system to the allergen, the more responsibly one should treat the doctor’s prescriptions. This is due to the fact that with this type of rhinitis, acute and severe immune reactions can develop, requiring emergency medical attention. Therefore, it is imperative to comply with all the doctor’s recommendations regarding taking the necessary drugs and actions that must be taken if the patient’s condition has worsened.
Prognosis
The prognosis of allergic rhinitis depends on many factors: the individual condition of the immune system of the patient, the environmental conditions, the timeliness of diagnosis and the adequacy of the therapy. However, as a rule, the prognosis is favorable. At observance of recommendations on creation of hypoallergenic regime and regular reception of therapy prescribed by a doctor, clinical manifestations of the disease and its possible complications decrease, and also the risk of expansion of the spectrum of sensitization is reduced.
With the timely start of treatment, relief can come quite quickly – usually within a few hours. If against the background of ongoing therapy for several days there is no desired effect, it is necessary to find out whether the diagnosis is correct, whether the drugs and dosage are chosen correctly, whether the patient follows all the recommendations correctly.
Prevention
Prevention of allergic rhinitis includes:
Removal of the causative allergen: elimination of items that collect a lot of dust (carpets, abundance of soft toys, open books, home flowers); replacement of bedding with artificial materials and rejection of down, feather, latex, buckwheat, wool, etc.; frequent change of bed linen; rejection of keeping pets in the apartment, etc. People with seasonal allergic rhinitis are advised to wear sunglasses and special nasal filters during flowering periods. Do not use phytotherapy, do not use honey. Be aware of possible cross food reactions.
- Participate in educational programs for patients (allergy schools).
- Adherence to a hypoallergenic diet, taking into account the sensitization spectrum.
- Exclusion of contact with non-specific irritants (tobacco smoke, exhaust gases, etc.)
- Prevention of respiratory infections.
- Caution in case of a severe allergy history and follow-up with an allergist over time.
- Early diagnosis of allergic diseases with exclusion of the diagnosis “bronchial asthma” in patients with allergic rhinitis.
- Timely preventive and basic therapy to eliminate the disease and prevent its complications.
- Timely implementation of ASIT therapy.
Allergic Rhinitis Facts
The basis of the pathology is an allergic reaction of type 1, also called an immediate reaction (anaphylactic, IgE-dependent type). Exposure to allergens results in the synthesis of specific antibodies – immunoglobulin E (IgE) and their fixation on mast cells and basophils. Repeated contact of immunoglobulin E-labeled mast cells with the allergen leads to excessive activation of these cells and release of biologically active substances from them. As a result, and there is a clinic of allergic rhinitis.
Allergic rhinitis is one of the most widespread diseases, it affects 10-20% of all population. In the U.S. the disease occurs in 20-40 million people, the prevalence among the pediatric population reaches 40%. Boys suffer more often. The incidence of allergic rhinitis is low in the age group up to 5 years old, and the disease rate rises at the early school age.
Increased urbanization, climate change and increased standard of living have created conditions for high allergenic loads and increased number of allergic diseases.
One of the most important problems associated with allergic rhinitis is late diagnosis. For example, 12% of patients are diagnosed in the first year of the disease, 50% in the first 5 years of the disease, and 38% will live with the disease for more than 10 years from its onset without a diagnosis. Late diagnosis leads to the development of complications of allergic rhinitis, and also significantly worsens the quality of life of the patient. Allergic rhinitis can start at any age, even in children of the first year of life.
Studies have shown that vaccination does not cause allergic disease. There is also evidence that the use of antibiotics in the first 5 years of life is not associated with the risk of asthma and allergic rhinitis.
Is allergic rhinitis lifelong?
Unfortunately, allergic rhinitis is a life-long illness with no known treatment. There are, however, a variety of therapy alternatives available to assist control symptoms. These may include avoiding allergens as much as possible, taking antihistamines or nasal corticosteroids, and undergoing immunotherapy via allergy injections or sublingual immunotherapy treatment. Working with a healthcare specialist to determine the appropriate treatment strategy for allergic rhinitis symptoms is critical.
Why is my allergic rhinitis not going away?
If you’ve been experiencing symptoms of allergic rhinitis that don’t seem to be going away, you may be wondering why. Allergic rhinitis is a chronic condition that can be caused by a number of allergens, including pollen, dust mites, and animal dander. In some cases, the symptoms of allergic rhinitis can persist even when allergens are avoided, or when over-the-counter medications are used. This could be due to a number of factors, such as environmental pollution, hormonal changes, or underlying medical conditions. It’s important to see a healthcare provider to determine the underlying cause of your symptoms and to develop an appropriate treatment plan. With the right treatment, you can manage your symptoms and enjoy a better quality of life.
Does vitamin C help allergic rhinitis?
According to research, vitamin C may help relieve allergic rhinitis symptoms such as itching, sneezing, and a runny or stuffy nose. Vitamin C is a natural antihistamine and antioxidant that helps decrease swelling and inflammation at the site of an allergic response. A high dosage of vitamin C alleviated allergy symptoms in 97% of participants in a trial of adults with skin or respiratory system allergies. It is crucial to emphasize, however, that vitamin C should not be used as a replacement for medical treatment, and people with severe allergies should seek medical advice before trying a supplementary therapy. Citrus fruits, kiwis, red bell peppers, and potatoes are all good sources of vitamin C.