Lung mild bibasilar atelectasis is the airlessness of lung tissue caused by the collapse of alveoli in a limited area (segment or lobe) or in the entire lung. The affected part of the lung is excluded from gas exchange, which may lead to signs of respiratory failure such as shortness of breath, chest pain, and a bluish skin tone.
Bibasilar atelectasis is usually detected through auscultation, chest X-ray, or CT scan of the lungs. These methods help reveal areas where the lung tissue has collapsed. Depending on severity, treatment may involve therapeutic bronchoscopy, physical therapy, chest massage, or anti-inflammatory medication. In rare cases, surgical removal of the affected area is required ⧉.
Normally, the lungs expand and contract about 20 times per minute, maintaining the body’s oxygen balance. In bibasilar atelectasis, however, the lower lung segments collapse, interrupting this process. The condition is more common after surgery, with lung injuries, or in overweight individuals ⧉.
Essentially, the alveoli—tiny air sacs in the lungs—deflate and lose air, leading to reduced oxygen exchange and difficulty breathing. Mild forms are usually reversible with prompt treatment and respiratory care ⧉.
What does mild bibasilar atelectasis mean
In medical terms, bibasilar atelectasis meaning describes a partial or complete collapse of a lung or both lungs. We have two lungs — the left and the right — both containing lobes. The left lung has two lobes, and the right lung has 3 lobes.
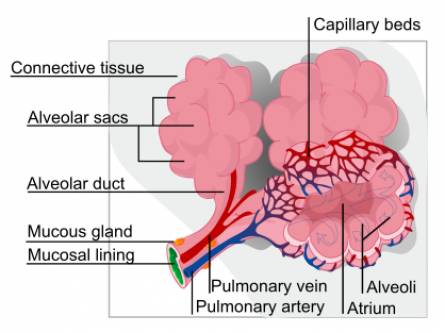
There are tiny air sacs formed like balloons containing blood vessels organized in clusters throughout the lungs.
These are called alveoli, which abnormally deflate due to an obstruction of the airflow with bibasilar atelectasis. It impacts the bottom portions of the lungs. The lethal result occurs from an absence of oxygen reaching crucial organs of the body.
Although it resembles pneumothorax, bibasilar atelectasis is caused by different conditions and circumstances. Pneumothorax can result in bibasilar atelectasis.
Causes of Bibasilar Atelectasis
Bibasilar atelectasis doesn’t just appear out of nowhere — it’s a reaction to something that blocks or limits airflow deep inside the lungs. Think of your lungs like a pair of balloons: if part of one balloon gets pinched or filled with fluid, it can’t expand properly. The same happens with the lower lobes of the lungs, which are more prone to collapse due to gravity and reduced ventilation.
Below are the main reasons this happens — and what’s actually going on inside the chest.
Blood Clot
A blood clot or internal bleeding within the lungs can block the air passages or fill tiny alveoli with blood. It’s like trying to inflate a sponge that’s already soaked — no air can enter. This often happens after blunt chest trauma, such as a car accident, when small vessels rupture and leak blood into the lung tissue ⧉.
Anesthesia
During surgery, anesthetic medications slow down breathing and relax the chest muscles. The lungs inflate less deeply, and the bottom sections — the bibasilar areas — don’t get enough air. Imagine leaving a balloon half-inflated for hours; parts of it stick together and lose elasticity. That’s essentially what happens during long surgeries. It’s one of the most common postoperative causes of mild atelectasis ⧉.
Foreign Body
Sometimes, a foreign particle or allergen can sneak into the airway — from food crumbs to dust or small toy parts in children. When that happens, the airflow behind the obstruction stops, and the air already inside gets slowly absorbed by the body. The lung tissue collapses, much like a balloon losing air through a knot you can’t untie.
Mucus Plug
After surgery or during respiratory infections, mucus can build up and thicken inside the bronchi. Since anesthesia and bed rest reduce the body’s natural cough reflex, this sticky plug becomes a literal cork in the airways. Doctors often remove it using suction, but deep-breathing exercises and coughing techniques are key to preventing it from returning — especially for people with asthma or cystic fibrosis ⧉.
Airway Narrowing
Chronic infections like tuberculosis or fungal inflammation can scar the airways, narrowing them over time. Picture a garden hose that’s been bent too many times — the water (or in this case, air) just can’t pass through freely. These structural changes can make certain lung segments, especially at the bases, collapse more easily.
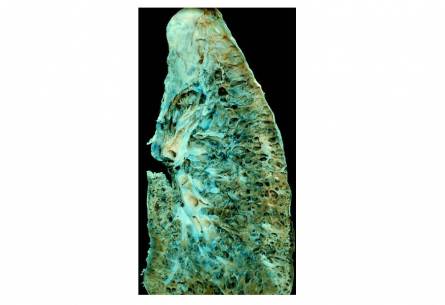
Lung Damage
Conditions such as chronic obstructive pulmonary disease (COPD) or pneumonia can weaken and damage the lung walls. When this happens, air can escape into the pleural space — the thin gap between the lungs and chest wall — leading to partial collapse. In medical terms, it’s like losing the seal on a tire: the air slowly leaks out, and the pressure that keeps the lung open is lost.
Trauma
A direct chest injury — from a car crash, fall, or even forceful sports impact — can compress or bruise the lung tissue. The bruised section may lose its ability to expand, creating a small pocket of collapse. In more serious trauma, broken ribs can press into the lung and make breathing both painful and shallow, worsening the effect.
Other Contributing Factors
Other situations that restrict deep breathing, such as lung tumors, obesity, prolonged bed rest, or heavy use of cough suppressants, can also set the stage for bibasilar atelectasis. Obesity, for example, increases abdominal pressure, making it harder for the diaphragm to move freely — so the lungs never fully inflate.
Atelectasis often develops after surgery. It is not typically life-threatening, but in some cases, it needs to be treated quickly.
my.clevelandclinic.org
Symptoms of Bibasilar Atelectasis

In most cases, mild bibasilar atelectasis affects only a small portion of the lower lungs, so it often goes unnoticed and symptom-free. The lungs are incredibly adaptive — even if part of the lower lobe collapses, the remaining healthy tissue usually compensates.
However, when a larger section or an entire lobe is involved, symptoms can become more pronounced. Because the collapsed alveoli stop exchanging oxygen properly, the body begins to show warning signs that something’s off ⧉.
Common symptoms include:
- Chest pain or tightness, often worse during deep breathing
- Wheezing or a whistling sound while breathing
- Persistent cough that may produce thick sputum
- Fever, especially if infection develops in the collapsed area
- Shortness of breath or a feeling of “can’t get enough air”
- Reduced chest expansion on the affected side
- Bluish or pale skin tone (a sign of low oxygen)
- Rapid heartbeat (tachycardia) as the body tries to deliver more oxygen
- Anxiety or restlessness, commonly linked to breathing discomfort
These symptoms can vary from barely noticeable to quite distressing, depending on how much of the lung is collapsed and whether there’s an underlying disease such as COPD or pneumonia ⧉.
Is Mild Bibasilar Atelectasis Serious?
Usually, no — mild bibasilar atelectasis isn’t life-threatening and often resolves with proper breathing exercises, hydration, and gentle activity. However, if left untreated or combined with an unhealthy lifestyle (such as physical inactivity or chronic lung disease), it can progress and create fertile ground for infections like pneumonia ⧉.
As Reyus Mammadli, medical consultant, notes:
“Even mild atelectasis is the body’s way of saying, ‘Take care of your lungs.’ Recovery begins with movement, breathing, and early attention to any warning signs.”
The following table compares the symptoms of bibasilar atelectasis and pneumonia:
| Symptoms | Bibasilar Atelectasis | Pneumonia |
|---|---|---|
| Coughing | Present, but usually less severe | Persistent and often accompanied by phlegm |
| Chest pain | Occasional discomfort or pressure | Sharp or stabbing pain that worsens with breathing or coughing |
| Shortness of breath | Mild to moderate, more noticeable with physical exertion | Severe and persistent, even at rest |
| Fatigue | Can occur but is not usually a primary symptom | Common and often accompanied by weakness |
| Fever | Rare | Common, often accompanied by chills and sweats |
| Breathing Sounds | Decreased breath sounds | Crackling or wheezing sounds during inhalation and exhalation |
| Causes | Obstructed airways, surgery, or lung diseases | Bacterial, viral, or fungal infections |
Bibasilar Atelectasis Diagnosis
Considering that physicians might misdiagnose bibasilar atelectasis as pneumothorax, a proper diagnosis needs explicit screening. You can expect a complete blood count test, a performance test of the kidneys, serum electrolytes check, and a physical examination.
Imaging tests might be bought and include chest x-rays to discover a collapsed lung, a chest computerized tomography scan, and a lung function test. A bronchoscopy may also be performed to figure out if an obstruction such as a tumor is present.
Mild Bibasilar Atelectasis Treatment
Bibasilar Atelectasis Treatment
Treatment for bibasilar atelectasis aims to re-expand the collapsed lung tissue, restore proper airflow, and prevent complications such as pneumonia. The approach depends on how severe the collapse is and what caused it — whether it’s mucus buildup, surgery, or an underlying lung disease.
1. Breathing Exercises and Physiotherapy
For mild cases, the cornerstone of treatment involves breathing exercises, incentive spirometry, and chest physiotherapy. These help reopen the alveoli — the tiny air sacs responsible for gas exchange.
- Incentive spirometer: a handheld device that encourages deep inhalation by providing visual feedback. Using it several times a day strengthens the lungs and helps them expand naturally.
- Postural drainage: positioning the patient so gravity assists in draining mucus from different parts of the lungs.
- Chest percussion and vibration: gentle tapping on the chest to loosen mucus and make it easier to cough up.
Reyus Mammadli, medical consultant, recommends combining these exercises with gentle physical activity: “Even walking a few steps or sitting upright can make a difference in lung expansion.”
2. Medication and Airway Clearance
If mucus plugs or inflammation are present, doctors often prescribe mucolytic agents (to thin mucus), bronchodilators (to open airways), or anti-inflammatory medications. In some cases, nebulized saline is used to moisten the airways and improve mucus clearance.
Patients with bacterial infection may receive antibiotics to prevent or treat pneumonia ⚩.
3. Bronchoscopy
When mucus, blood clots, or foreign objects block airflow, doctors may perform a bronchoscopy. This minimally invasive procedure uses a thin, flexible tube with a camera to visualize the airways and remove obstructions.
Bronchoscopy has a high success rate (about 8–9 out of 10 cases) for resolving localized atelectasis ⚩. It’s performed under mild sedation and typically takes less than an hour.
4. Positive Pressure and Oxygen Therapy
In hospital settings, positive pressure ventilation (CPAP or BiPAP) may be used to gently force air into the lungs, keeping the alveoli open. Supplemental oxygen therapy is often prescribed to stabilize oxygen levels while the lungs recover.
These methods are particularly effective in patients with post-surgical atelectasis or chronic respiratory conditions.
5. Surgery (in Severe or Chronic Cases)
When conservative treatment fails or when there’s irreversible lung damage, surgical removal (resection) of the affected segment may be necessary. This is rare and typically reserved for patients with long-term scarring or recurrent lung collapse due to tumors.
6. Lifestyle and At-Home Support
Recovery doesn’t end at the hospital. Patients are encouraged to:
- Stay mobile – even short walks stimulate lung expansion.
- Maintain hydration – water helps thin mucus for easier clearance.
- Use proper posture – sitting upright supports better breathing mechanics.
- Avoid cough suppressants unless prescribed, as coughing helps clear airways.
Editorial Advice
According to Reyus Mammadli, medical consultant, the key to managing bibasilar atelectasis is consistency:
“The lungs are remarkably resilient. With steady breathing exercises, early mobilization, and proper medical follow-up, most cases improve within days.”
In short, mild bibasilar atelectasis is highly treatable, especially when addressed early with a mix of physiotherapy, medication, and active recovery practices.
Bibasilar Atelectasis Prevention
You can prevent bibasilar atelectasis by not ingesting foreign items and preventing the use of tobacco (don’t smoke!), too making use of anesthetic vices when it is not required.
Considering that numerous cases are not preventable due to existing health conditions and surgeries, there are steps to lower risk of bibasilar atelectasis complications that include:
- Doing deep breathing exercises routinely.
- Using favorable expiratory pressure devices to help in breathing when needed.
- Recording symptoms and breathing patterns.
- Preserving positions that promote mucus drainage.
Bibasilar atelectasis can be a frightening condition that might result in a total lung collapse in extreme cases. Seen mainly in post-surgical recovery, using anesthetics can greatly affect lung working and airway passages.
Health conditions and injury to the lungs can likewise bring upon bibasilar atelectasis. Mild conditions do not require treatment while more serious cases require surgery.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.