Multiple Sclerosis is one of the most common diseases associated with a violation of the human immune system. To cope with the severe consequences of this disease, it is necessary to determine its signs as soon as possible and begin appropriate treatment.
What is Multiple Sclerosis?
Multiple sclerosis (MS) is a progressive, immune-mediated condition. That implies the system created to keep your body healthy wrongly attacks parts of your body that are crucial to daily function. The protective coverings of afferent neuron are damaged, which causes reduced function in the brain and spine.
MS is a disease with unforeseeable symptoms that can vary in intensity. While some individuals experience tiredness and numbness, extreme cases of MS can cause paralysis, vision loss, and reduced brain function.
Common Symptoms of Multiple Sclerosis
Typical early signs of multiple sclerosis (MS) include:
- vision problems
- tingling and numbness
- pains and spasms
- weak point or fatigue
- balance problems or dizziness
- bladder concerns
- sexual dysfunction
- cognitive problems
For many individuals, the first brush with what’s later on detected as MS is what medical professionals call clinically isolated syndrome (CIS). This episode of neurological symptoms typically lasts 24 hours. It happens when your body immune system wrongly informs your body to attack myelin, the protective sheath over afferent neuron in your brain and spine. You may hear your medical professional call this demyelination. It triggers scars, or lesions, that make it harder for signals to take a trip in between your brain and your body.
There are two types of CIS:
- Monofocal episode: You have one sign.
- Multifocal episode: You have more than one sign.
Vision problems
Visual issues are one of the most typical symptoms of MS. Inflammation impacts the optic nerve and interferes with central vision. This can cause blurred vision, double vision, or loss of vision.
You may not discover the vision problems right away, as degeneration of clear vision can be sluggish. Pain when you look up or to one side also can accompany vision loss. There are variety of ways to cope with MS-related vision changes.
Tingling and numbness
MS impacts nerves in the brain and spine (the body’s message center). This implies it can send out conflicting signals around the body. Often, no signals are sent out. This leads to numbness.
Tingling experiences and numbness are one of the most common warning signs of MS. Common websites of numbness consist of the face, arms, legs, and fingers.
Pain and spasms
Chronic pain and involuntary muscle spasms are also common with MS. One study, according to the National MS Society, revealed that half of individuals with MS had chronic pain.
Muscle stiffness or spasms (spasticity) are likewise common. You may experience stiff muscles or joints as well as uncontrollable, unpleasant jerking movements of the extremities. The legs are usually impacted, but back pain is likewise common.
Fatigue and weakness
Inexplicable tiredness and weak point impact about 80 percent of individuals in the early stages of MS.
Chronic fatigue takes place when nerves degrade in the spinal column. Normally, the fatigue appears suddenly and lasts for weeks prior to enhancing. The weak point is most obvious in the legs in the beginning.
Balance issues and dizziness
Dizziness and issues with coordination and balance can decrease the movement of someone with MS. Your medical professional may refer to these as issues with your gait. Individuals with MS typically feel lightheaded, dizzy, or as if their surroundings are spinning (vertigo). This sign often occurs when you stand up.
Bladder and bowel dysfunction
A dysfunctional bladder is another sign occurring in as much as 80 percent of people with MS. This can include regular urination, strong urges to urinate, or inability to keep in urine.
Urinary-related symptoms are often workable. Less frequently, people with MS experience constipation, diarrhea, or loss of bowel control.
Sexual dysfunction
Sexual arousal can likewise be a problem for people with MS due to the fact that it begins in the central nerve system– where MS attacks.
Cognitive issues
About half of people with MS will develop some type of problem with their cognitive function. This can include:
- memory issues
- shortened attention span
- language problems
- difficulty remaining arranged
Anxiety and other psychological health issue are likewise typical.
Changes in emotional health
Major anxiety prevails amongst people with MS. The tensions of MS can also cause irritability, mood swings, and a condition called pseudobulbar affect. This includes bouts of unmanageable weeping and chuckling.
Coping with MS symptoms, along with relationship or family issues, can make depression and other psychological conditions much more challenging.
Other symptoms
Not everybody with MS will have the same symptoms. Various symptoms can manifest during relapses or attacks. Along with the symptoms mentioned on the previous slides, MS can also cause:
- hearing loss
- seizures
- uncontrollable shaking
- breathing problems
- slurred speech
- trouble swallowing
Is MS hereditary?
MS isn’t necessarily hereditary. However, you have a higher chance of establishing the disease if you have a close relative with MS, according to the National MS Society.
The general population just has 0.1 percent chance of establishing MS. But the number leaps to 2.5 to 5 percent if you have a sibling or parent with MS.
Heredity isn’t the only consider identifying MS. A twin only has a 25 percent possibility of establishing MS if their twin has the disease. While genes is certainly a threat aspect, it’s not the only one.
Symptoms of MS in Women
According to the National Multiple Sclerosis Society (NMSS), at least 2 or 3 times more women than men get a medical diagnosis of MS.
Overall, MS seems to affect men and women similarly. Nevertheless, a doctor can not anticipate which symptoms somebody with MS will get, the severity of the symptoms, or the progression of the disease.
The factor for this is that the disease assaults the myelin arbitrarily, and the nerves that it impacts can vary from person to individual.
Although males and females with MS often experience similar symptoms, certain factors, such as menstruation, pregnancy, and menopause, might influence MS symptoms in women.
Hormone effects
There is some proof to suggest that MS can affect women in a different way than men due to hormonal changes, consisting of those that take place during:
Menstruation
More research is needed to draw firm conclusions, but the NMSS state that some research studies have actually found that women with MS have worse symptoms within a week of starting their period.
Research studies that utilized an MRI have also shown that MS disease activity may change according to the different hormonal levels throughout menstruation.
Pregnancy
Pregnancy can decrease the danger of MS sign flare-ups, especially during the 2nd and third trimesters.
Scientists believe that pregnancy has a protective result against MS by raising the levels of compounds that help in reducing inflammation and the impacts of the disease.
Women who are pregnant likewise have naturally higher levels of distributing corticosteroids, another type of immunosuppressant.
Although pregnancy can temporarily lower some MS symptoms, flare-ups tend to return in the first 3 to 6 months postpartum. Nevertheless, in the long term, there is no proven link between pregnancy and a higher danger of impairment.
While being pregnant can temporarily decrease the danger of flare-ups, pregnancy likewise puts a great deal of physical stress on the body, which can make certain symptoms of MS even worse.
In addition, a few of the medications that individuals use for MS are not safe to take throughout pregnancy and can aggravate symptoms.
Anyone with MS who is pregnant or preparing to become pregnant need to discuss their medications with their medical professional.
Some MS symptoms that pregnancy typically intensifies include:
- fatigue
- gait issues
- bladder and bowel problems
Menopause
MS symptoms might intensify after menopause, perhaps because decreasing estrogen levels negatively impact disease progression.
However, it is hard to inform whether MS symptoms aggravate due to the fact that of menopause or simply as a natural outcome of aging or the progression of the condition.
A lot more research study is required to understand the relationship in between menopause and MS symptoms.
Diagnosis
A doctor– more than likely a neurologist– will carry out a number of tests to detect MS, consisting of:
- neurological test: your doctor will look for impaired nerve function
- eye exam: a series of tests to assess your vision and look for eye diseases
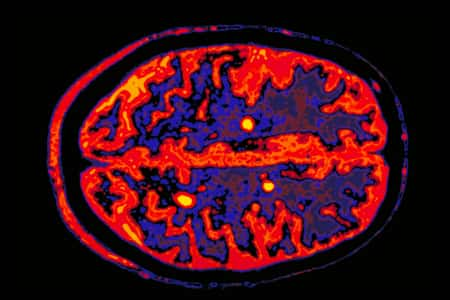
- magnetic resonance imaging (MRI): a method that utilizes an effective electromagnetic field and radio waves to develop cross-sectional images of the brain and spinal cord
- back tap (also called a back leak): a test including a long needle that’s inserted into your spine to remove a sample of fluid distributing around your brain and spinal cord
Doctors use these tests to search for damage to the central nervous system in 2 separate areas. They need to likewise determine that a minimum of one month has actually passed in between the episodes that triggered damage. These tests are also utilized to eliminate other conditions.
MS often astonishes doctors due to the fact that of how much it can vary in both its intensity and the manner ins which it affects individuals. Attacks can last a few weeks and then vanish. Nevertheless, relapses can get gradually even worse and more unforeseeable, and come with various symptoms. Early detection may assist avoid MS from progressing rapidly.
Misdiagnosis
Misdiagnosis is likewise possible. A study found that almost 75 percent of surveyed MS specialists had actually seen at least 3 patients over the previous 12 months who had been misdiagnosed.
Treatment for Multiple Sclerosis
MS is a challenging disorder, but researchers have actually found numerous treatments that can slow its progression.
The very best defense versus MS is seeing your doctor instantly after you experience the first indication. This is especially essential if somebody in your immediate family has the disorder, as it’s one of the key threat elements for MS.
Multiple Sclerosis: Question and Answers
What is the prognosis of multiple sclerosis (MS)?
If left neglected, more than 30% of patients with MS will develop significant physical disability within 20-25 years after beginning. Numerous of the disease-modifying agents used in MS have slowed special needs progression within the duration of research trials; whether these impacts will be kept over longer periods is not known.
Less than 5-10% of patients have a medically milder MS phenotype, in which no considerable physical disability collects in spite of the passage of several decades after onset (in some cases in spite of multiple new sores seen on MRI). Detailed examination of these patients in numerous instances reveals some degree of cognitive wear and tear.
Male patients with primary progressive MS have the worst prognosis, with less favorable action to treatment and quickly building up special needs. The greater occurrence of spinal cord sores in main progressive MS is likewise a factor in the rapid development of special needs.
What is the life expectancy of patients with multiple sclerosis (MS)?
Life expectancy is reduced only slightly in persons with MS, and the survival rate is linked to special needs. Death generally results from secondary complications (50-66%), such as pulmonary or renal causes, however can also be because of primary problems, suicide, and triggers unrelated to MS. The Marburg variant of MS is an acute and clinically fulminant type of the disease that can cause coma or death within days.
How is constipation defined in multiple sclerosis (MS)?
Constipation is the most frequent bowel complaint in patients with MS and is characterized as the infrequent or hard passage of stools. Constipation might be the result of a neurogenic bowel or of immobility, which results in slowed bowel activity. In addition, patients who have actually limited their fluid consumption in an effort to handle bladder symptoms and those with limited access to fluids due to immobility tend to have dry difficult stools.
How does multiple sclerosis (MS) present?
Presentation of MS frequently varies among patients. Some patients have a predominance of cognitive changes, while others present with prominent ataxia, hemiparesis or paraparesis, anxiety, or visual symptoms. In addition, it is important to acknowledge that the development of physical and cognitive impairment in MS may take place in the lack of clinical exacerbations.
What are the common symptoms of multiple sclerosis (MS)?
Traditional MS symptoms are as follows:
- Sensory loss (ie, paresthesias) – Usually an early grievance
- Spinal cord symptoms (motor) – Muscle cramping secondary to spasticity
- Spine symptoms (free) – Bladder, bowel, and sexual dysfunction
- Cerebellar symptoms – Charcot triad of dysarthria (scanning speech), nystagmus, and intention tremor
- Optic neuritis
- Trigeminal neuralgia – Bilateral facial weakness or trigeminal neuralgia
- Facial myokymia (irregular twitching of the facial muscles) – May also be a presenting symptom
- Eye symptoms – Including diplopia on lateral look; these occur in 33% of patients
- Heat intolerance
- Constitutional symptoms – specifically tiredness (which occurs in 70% of cases) and lightheadedness; tiredness needs to be distinguished from depression (which may, however, exist side-by-side), lack of sleep, and exertional fatigue due to special needs
- Pain – Occurs in 30– 50% of patients at some point in their illness
- Subjective cognitive difficulties – With regard to attention period, concentration, memory, and judgment
- Depression – A common symptom
- Ecstasy – Less common than anxiety
- Bipolar illness or frank dementia – May appear late in the disease course but is in some cases discovered at the time of initial diagnosis.
- Symptoms connected with partial acute transverse myelitis
What are unusual symptoms and signs of multiple sclerosis (MS)?
Patients with MS may provide with lots of other symptoms, consisting of the following:
- Aphasia or dysphasia (takes place very hardly ever).
- Seizures (5% of patients with MS).
- Other paroxysmal symptoms (eg, ataxia, akinesia, paresthesias, pruritus).
- Considerable motor problems without sensory deficits or dysautonomia.
Paroxysmal symptoms might occur in bouts and are frequently activated by movement or sensory stimuli.
What is the function of fatigue in multiple sclerosis (MS)?
Tiredness is one of the most typical sign of MS, reported by at least 75% of patients with the disease. Tiredness is referred to as a frustrating feeling of lassitude or lack of physical or psychological energy that hinders activities.
An approximated 50-60% of individuals with MS explain tiredness as one of their most annoying symptoms, and it is a major reason for joblessness amongst MS patients. One should eliminate comorbid medical conditions, such as infections, anemia, vitamin deficiencies (eg, vitamin B12, folic acid, vitamin D deficiency) or thyroid disease, before associating tiredness to MS.
How is pain identified in multiple sclerosis (MS)?
As formerly discussed, pain can be a typical occurrence in MS, with 30– 50% of patients experiencing it at a long time in the course of their disease. Pain generally is not associated with a less favorable prognosis, nor does it always impair function; however, because it can have considerable influence on lifestyle, it needs to be dealt with appropriately.
Pain in MS can be classified as main or secondary. Main pain is associated with the demyelinating procedure itself. This neuropathic pain is often identified as having a burning, gnawing, or shooting quality. Secondary pain in MS is primarily musculoskeletal in nature and possibly arises from poor posture, bad balance, or irregular use of muscles or joints as an outcome of spasticity.
How is bladder dysfunction defined in multiple sclerosis (MS)?
Urinary symptoms are common in MS, with a lot of patients experiencing problems at some time in their disease. Bladder issues are a source of significant morbidity, impacting the individual’s family, social, and work duties. Bladder dysfunction can be classified as failure to shop, failure to empty, or both. Patients with impaired storage have a little, spastic bladder with hypercontractility of the detrusor muscle. Symptoms experienced may include seriousness, frequency, incontinence, and nocturia. MS patients with advancing impairment and impaired bladder function might experience persistent urinary tract infections.
Which body systems are evaluated in the physical examination of multiple sclerosis (MS)?
An extensive physical exam, including neurologic evaluation, is important to identify deficits in MS. All systems should be addressed, including cognition, state of mind, motor, sensory, and musculoskeletal, as well as the following:.
- Reflexes.
- Coordination.
- Bulbar function.
- Vision.
- Gait.
- Skin.
Bulbar participation generally describes dysfunction of lower cranial nerves whose nuclei live in the lower brainstem. Symptoms consist of dysphagia, which does not occur frequently in early MS and so might be credited to a various disorder.
Which disability scale is most commonly used to rate the status of a client with multiple sclerosis (MS)?
A client might be ranked according to a number of medical special needs scales, on the basis of findings on the history and physical exam. The most commonly accepted of these is the 10-point Kurtzke Expanded Disability Status Scale (EDSS), which was developed originally in 1955 as the Disability Status Scale and has been revised over the years.
Why is early medical diagnosis of multiple sclerosis (MS) crucial?
Early medical diagnosis is important due to the fact that there is growing evidence that early intervention is useful. It is known through the work of Trapp et al that axonal loss can be present, even in asymptomatic patients, early in the disease process. In addition, research studies in patients with a first attack of neurologic symptoms suggestive of MS have actually demonstrated decreased special needs and lower secondary relapse rates with interferon treatment.
What are the McDonald requirements for a medical diagnosis of multiple sclerosis (MS)?
The McDonald requirements, which were established in 2001 by a global specialist panel and revised several times, most recently in 2017, offer recommendations on the diagnosis of MS, including diagnosis after a single attack. The criteria include a combination of medical, imaging, and paraclinical tests.
What are the advantages of MRI over CT scanning and scientific exam in multiple sclerosis (MS)?
MRI is more delicate for identifying active plaques than is double-dose computed tomography (CT) scanning or clinical assessment. MRI far surpasses CT scanning in the capability to demonstrate intramedullary pathology.
What do MRI results expose in multiple sclerosis (MS)?
MRI shows brain abnormalities in 90-95% of MS patients and spinal cord sores in as much as 75%, particularly in senior patients. T2-weighted images show edema and more chronic lesions, whereas T1-weighted images show cerebral atrophy and “great voids.” These black holes represent areas of axonal death.
According to new research study, tracking levels of iron in particular areas of the brain in patients with MS by utilizing unique MRI may track disease development and examine treatment effectiveness in medical trials. In the research study, a new strategy referred to as quantitative susceptibility mapping (QSM) recognized different iron patterns in the brains of patients with MS (N= 600) compared to healthy controls (N= 250). Patients with MS had lower iron material in the thalamus and greater iron content in other deep gray-matter structures compared with controls.
What are the functions of radiography, angiography, and ultrasonography in the examination of multiple sclerosis (MS)?
The arrival of MRI has restricted the role of CT and radiography in the diagnosis and treatment of MS. Occasionally, plain radiographs may be utilized to omit mechanical bony lesions.
Angiography likewise has a limited function, however may occasionally be considered when CNS vasculitis is part of the differential medical diagnosis in a patient with undifferentiated findings. No favorable angiographic findings are specific to MS.
Ultrasonography is not presently used in the examination of MS. However, Berg et al utilized transcranial ultrasonography to determine the size of the ventricles in patients with MS and found that increasing ventricular size is associated with the MRI-determined brain volume, in addition to with cognitive dysfunction and medical disability. Further research studies may establish a role for ultrasonography in identifying the prognosis and assisting treatment of patients with MS.
What are the 2 primary approaches to treatment for multiple sclerosis (MS)?
Treatment of multiple sclerosis (MS) has 2 aspects: immunomodulatory treatment (IMT) for the underlying immune disorder and therapies to alleviate or modify symptoms. IMT is directed toward reducing the frequency of regressions and slowing progression. Currently, most disease-modifying agents have been authorized for use only in relapsing forms of MS. Mitoxantrone (see below) is likewise approved for the treatment of secondary (long-lasting) progressive and progressive relapsing MS.
What is the treatment for scientifically separated syndrome (CIS), and what are the implications for the advancement of multiple sclerosis (MS)?
In the research study, 618 patients were dealt with either with teriflunomide in dosages of 14 mg or 7 mg each day or placebo. Patients were consisted of if they experienced a first acute or subacute distinct neurologic event consistent with demyelination, start of MS symptoms within 90 days of randomization, and MRI showing 2 or more attributes of MS. During 2 years of treatment, patients getting 14 mg of teriflunomide experienced a 43% decrease in the danger for conversion to medically certain MS compared to placebo. Patients who got 7 mg of the drug per day had a 37% reduction in the danger for conversion vs placebo.
Given the large spectrum of medical symptoms that MS can produce, patients might need assessments with a range of specialists. Undoubtedly, patients with MS are frequently best served by a multidisciplinary approach.
What treatments are offered for acute regressions of multiple sclerosis (MS)?
Methylprednisolone (Solu-Medrol) can hasten recovery from an acute worsening of MS. There is no clear proof that it changes the general disease progression.
Plasma exchange (plasmapheresis) can be used short-term for extreme attacks if steroids are contraindicated or ineffective. The 2011 AAN guideline for plasmapheresis in neurological diseases categorizes plasmapheresis as “most likely effective” as second-line treatment for falling back MS exacerbations that do not react to steroids.
Texts commonly explain anti-inflammatory treatment as an option for acute transverse myelitis and acute disseminated sleeping sickness; however, very few supporting information are provided. Dexamethasone is frequently used. Anti-inflammatory treatment for ON is very controversial.
Which medications are used to treat spasticity in multiple sclerosis (MS), and what are the standard does and side effects?
Dantrolene sodium (Dantrium) acts straight on skeletal muscle to reduce spasticity. This agent is used less frequently than baclofen due to the fact that of its hepatotoxicity at higher doses and numerous drug interactions.
The anticonvulsant drug gabapentin (Neurontin) is particularly helpful in patients who experience spasticity and neuropathic pain. It is easily titrated from 300 to 3600 mg/day in divided dosages. Nevertheless, in addition to being reasonably costly, gabapentin typically triggers considerable sedation, which is successfully dosage limiting.
Tizanidine (Zanaflex), a centrally acting alpha-adrenergic agonist, is also utilized to manage spasticity. Tizanidine has effects similar to those of baclofen, however it produces less weakness and more sedation. This drug is titrated from 2 to 32 mg/day in divided dosages.
Additional treatments for serious spasticity management consist of intramuscular botulinum toxin, phenol nerve blocks, and intrathecal baclofen pump placement. Since of their higher invasiveness, these treatments are usually reserved for the most challenging cases.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.