The pancreas, a glandular organ hidden beneath the stomach, can develop a malignant tumor known as pancreatic cancer. Pancreatic cancer, which is among the deadliest and has a low survival rate, is very frequently not discovered until it has spread to other organs in the body.
We will look at the causes, risk factors, warning signs, diagnostic procedures, and therapies for pancreatic cancer in this blog article.
Together with options for assistance, we will also give advice on how to handle a pancreatic cancer diagnosis.
We hope that this blog article will provide you with more knowledge and understanding as you travel this challenging road, whether you have been diagnosed with pancreatic cancer or you are a caretaker for someone who has.
What is Pancreatic Cancer?
A tumor is created when cells in the pancreas, a gland beneath the stomach, begin to expand and divide uncontrolled. This is how pancreatic cancer develops. In order to help the body properly digest food, the pancreas generates hormones and digestive fluids.
The pancreas’ healthy cells have the potential to accumulate and become malignant growths when they cease to function normally and multiply uncontrollably. There are several different kinds of pancreatic cancer, with pancreatic adenocarcinoma accounting for over 95% of occurrences. It is a very aggressive malignancy with a bad prognosis that is frequently challenging to identify early on.
To provide readers a thorough understanding of this condition, we will explore a number of issues in this blog part, including the many forms of pancreatic cancer, its symptoms, diagnoses, therapies, and risk factors.
Types of Pancreatic Cancer
Exocrine tumors and endocrine tumors are the two primary categories used to describe pancreatic cancer. Almost 90% of all pancreatic cancers are exocrine tumors, the most frequent kind. The most prevalent kind of exocrine tumor is pancreatic ductal adenocarcinoma. The pancreatic ducts’ glandular tissue, which lines them, is where this cancer grows.
Conversely, endocrine tumors, also known as pancreatic neuroendocrine tumors (NETs), are uncommon, making for fewer than 5% of all pancreatic cancers. While PanNETs that are not active do not emit hormones, functioning PanNETs do, such as insulinomas and gastrinomas.
To develop the most successful treatment strategy, doctors must first accurately diagnose the type of pancreatic cancer a patient has. The symptoms, diagnosis, therapy, and prevention of pancreatic cancer will all be covered in the parts that follow.
Symptoms of Pancreatic Cancer
Once it has progressed to other organs, pancreatic cancer frequently stays undiagnosed. As there may be no symptoms at all in the early stages, this is one of the reasons why it is challenging to diagnose.
Yet, when the cancer worsens, a few typical symptoms start to show themselves. They include back or stomach discomfort, an inability to eat, weight loss, weariness, depressive symptoms, bloating, and nausea.
Jaundice, which is characterized by yellowing of the eyes and skin as well as darker urine and paler feces, may also occur in certain people.
It is crucial to consult a healthcare professional if you encounter any of these symptoms since they might be a sign of pancreatic cancer.
Don’t wait to get medical help if you are worried; early discovery and treatment can increase your chances of survival.
Diagnosing Pancreatic Cancer
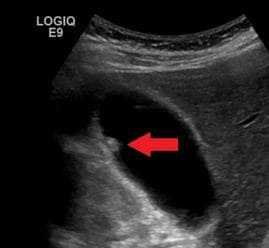
A critical first step in successfully treating pancreatic cancer is accurate diagnosis. Accurate pancreatic cancer diagnosis requires a mix of imaging studies and laboratory research. To pinpoint the exact position and size of the tumor, imaging procedures including CT scans, MRI scans, and endoscopic ultrasonography are performed.
Cancer-related chemicals known as tumor markers, such as CA19-9, can also be found via blood testing. Analyzing a biopsied tissue sample is the most precise approach to identify pancreatic cancer.
Moreover, germline testing is now advised for anybody who has been given a pancreatic cancer diagnosis. With the purpose of finding any biliary blockage, laboratory testing such complete blood counts and liver enzyme analyses are also carried out. As the signs of pancreatic cancer are sometimes ambiguous and nonspecific, early detection is difficult, but it improves the odds of effective therapy.
For a better chance of detecting pancreatic cancer in its early stages, it is critical to be aware of the risk factors, symptoms, and early detection methods, including screening tests.
Treatments for Pancreatic Cancer
Chemotherapy, radiation, and surgery are the three major forms of treatment for pancreatic cancer. Chemotherapy, which can be used alone or in combination with targeted therapy or immunotherapy, is frequently the initial line of treatment for pancreatic cancer. To destroy cancer cells, chemotherapy and radiation are used together in chemoradiation treatment.
Surgery could be a possibility if the cancer has not metastasized outside of the pancreas. Surgery is less successful for pancreatic cancer since it is frequently detected after it has spread and is frequently identified late.
Another therapy choice is palliative care, which focuses on symptom relief and enhancing quality of life. To establish the best course of action for certain pancreatic cancer situations, it’s crucial to consult with a trained healthcare practitioner.
Most effective medications used to treat pancreatic cancer
- FOLFIRINOX: The most effective first-line chemotherapy combination for pancreatic cancer includes oxaliplatin, folinic acid, irinotecan, and fluorouracil, known as FOLFIRINOX. This combination has shown to extend survival and improve outcomes for patients.
- Abraxane: Another promising drug in the treatment of pancreatic cancer is Abraxane, which uses a nanoparticle formulation of paclitaxel. This drug has shown to have fewer side effects than traditional chemotherapy and can be used with gemcitabine.
- Gemcitabine: Gemcitabine, also known as Gemzar, is a chemotherapy drug often used in combination with radiation therapy. It has been approved by the FDA for use in locally advanced, unresectable, or metastatic pancreatic cancer.
- Erlotinib: Erlotinib, in combination with gemcitabine, is also approved by the FDA as a first-line treatment for locally advanced, unresectable pancreatic cancer. This drug targets specific enzymes on the cancer cells, leading to improved outcomes.
- Somatostatin with Steroids: For advanced pancreatic cancer, somatostatin with steroids can be used to reduce swelling and blockages. This combination can help to alleviate symptoms and improve quality of life for these patients.
Prognosis and Survival Rates
When it comes to pancreatic cancer, the disease is frequently diagnosed after it has progressed. The prognosis may also worsen as a result, making therapy more challenging. In actuality, just 11% of people with pancreatic cancer in the United States survive the disease for five years.
Survival statistics, however, might be more optimistic for people who receive an early diagnosis, before the disease has progressed. Localized pancreatic cancer has a 44% 5-year relative survival rate.
Treatment can increase the median survival duration from 3 1/2 months to 8 months even in cases with advanced pancreatic cancer. It’s vital to keep in mind that these figures are still rising even though they may not appear encouraging.
Patients with pancreatic cancer now have a 5-year survival rate that has grown from 6% to 12% over the previous ten years, which shows that treatment choices have advanced significantly. The goal is that survival rates will continue to rise with more study and treatment developments.
Risk Factors for Pancreatic Cancer
The chance of acquiring pancreatic cancer is greatly influenced by risk factors. Age is a key risk factor for pancreatic cancer, as was established in the sections prior to this one. The majority of those who get the disease are above the age of 45.
Also, it has been demonstrated scientifically that factors that raise the risk of getting pancreatic cancer include cigarette smoking, chronic pancreatitis, being overweight, or engaging in little physical exercise.
Moreover, investigations have found a connection between pancreatic cancer and diabetes, gallstones, and family history. To prevent or identify pancreatic cancer at an early stage, it is essential to be aware of these risk factors, alter one’s lifestyle, and/or get routine tests, if necessary.
Prevention and Early Detection
Fighting pancreatic cancer requires prevention and early detection. There are actions people may do to lower their risk, even while some risk factors, such age, gender, race, and family history, cannot be managed. Keeping a healthy weight, giving up smoking and alcohol, and following a balanced diet can all help avoid.
Furthermore, improving outcomes for those with pancreatic cancer requires early diagnosis. Those at high risk due to a family history of the condition or genetic abnormalities can be examined, even though there is presently no reliable screening test for the general population.
A blood test that reveals elevated levels of the tumor marker CA19-9 may assist confirm a diagnosis. Recent research has revealed possible biomarkers that may help in early identification. It is crucial for people to discuss their risk and any prospective screening methods with their healthcare professionals.
Support and Resources for Pancreatic Cancer Patients
Patients and their families with pancreatic cancer need both medical care and emotional support. To assist persons impacted by pancreatic cancer in adjusting to their diagnosis, there are several organizations, support groups, books, and films available.
Information about support groups in every state is freely available from the Pancreatic Cancer Action Network. For people impacted by pancreatic cancer, CancerCare also provides free professional support services.
Only one organization, the National Pancreas Foundation, supports studies into pancreatic cancer, acute pancreatitis, chronic pancreatitis, and pediatric pancreatitis. Those who are coping with cancer can also get free and private phone support through the Macmillan Support Line.
Also, medical professionals may assist patients in organizing their emotions and coming up with coping mechanisms for their diagnoses. As individuals with pancreatic cancer navigate their treatment journey, these tools can assist in providing vital emotional support.
Latest Research and Breakthroughs in Pancreatic Cancer
The fight against pancreatic cancer has new hope thanks to recent developments in medical science. In February 2022, the Institute of Cancer Research revealed a discovery that suggested stroma-modifying medications might increase Whipple surgery patients’ chances of surviving by up to 40%.
Also, by specifically targeting the distinct metabolic pathways used by cancer cells, immunotherapy has demonstrated encouraging outcomes in the treatment of pancreatic cancer. Hematopoietic cell kinase (HCK) inhibitor research has shown that pancreatic cancers may respond better to therapy when this protein is targeted.
Also investigated as a potential therapeutic option is the combination of internal radiation and chemotherapy. Moreover, one of the medications being examined for the treatment of pancreatic cancer is the LAG3 inhibitor from Bristol Myers Squibb, which has previously received FDA approval for the treatment of other tumors.
Although there has clearly been progress, there is still a lot to be discovered about this contagious disease. Medical researchers are working to find new methods for identifying and treating pancreatic cancer, which will ultimately improve the prognosis for patients.