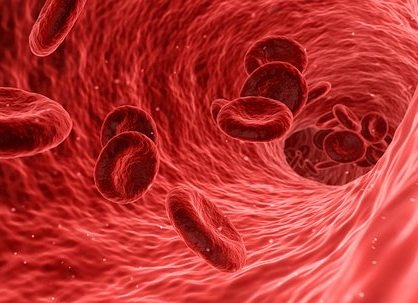
Sickle cell disease (SCD) is a serious group of conditions which are inherited (genetic). It affects the red blood cells in the blood. Sickle cell anaemia is the name of a specific form of SCD where there are two sickle cell genes.
What is Sickle Cell Disease?
With SCD, the red blood cells tend to go out of shape and become sickle-shaped (like a crescent moon) – rather of their regular disc shape. This can cause numerous problems. Between the episodes of disease, individuals with SCD feel well.
SCD is therefore a group of conditions that cause red cells to become sickle-shaped.
Sickle cell trait is not the same as SCD or sickle cell anaemia. Sickle cell characteristic implies you carry a sickle cell gene, however it does not usually cause disease.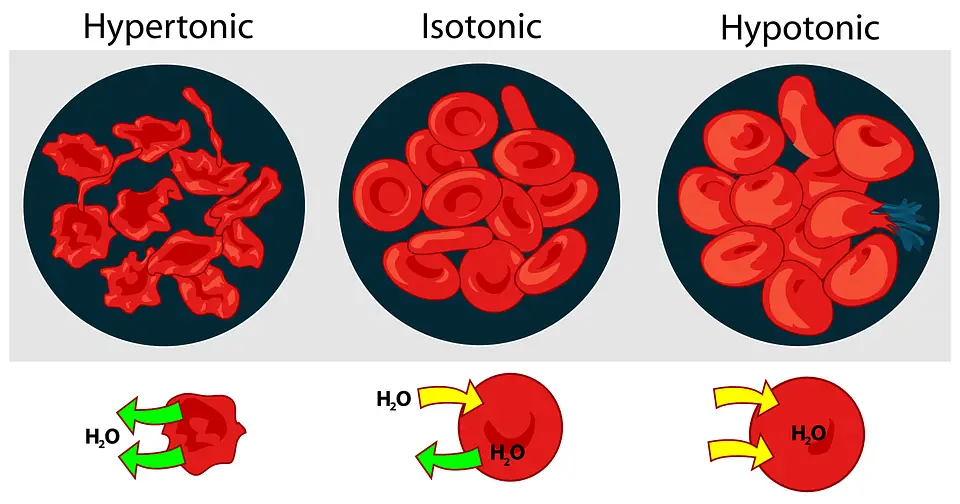
Who gets SCD?
In the UK, about 12,500 individuals have sickle cell disease. It is more typical in individuals whose family origins are African, African-Caribbean, Asian or Mediterranean. It is uncommon in individuals of North European origin. Usually, 1 in 2,400 babies born in England have SCD, however rates are much greater in some metropolitan areas – about 1 in 300 in some locations.
SCD is now one of the most typical acquired (hereditary) conditions in children born in the UK.
What Causes Sickle Cell Disease?
The cause is acquired (hereditary). It is a change in the genes which tell the body how to make an essential protein called haemoglobin. To obtain SCD, you have to have two transformed haemoglobin genes, one from each parent. If you just have one of these genes, you will have sickle cell characteristic, which is quite milder.
The most typical type of sickle cell disease is where you have two sickle cell genes (sickle cell anaemia). The medical shorthand for this is haemoglobin SS or HbSS. Other types of sickle cell disease involve one sickle cell gene plus another unusual haemoglobin gene of a different type. These include: haemoglobin SC; haemoglobin S/beta thalassaemia; haemoglobin S/Lepore; haemoglobin SO Arab.
The symptoms, diagnosis and treatment are comparable for all the sickle cell conditions.
How do the Sickle Cell Genes Cause SCD?
Sickle cell genes affect the production of an important chemical called haemoglobin. Haemoglobin lies in red blood cells, which belong to the blood. Haemoglobin carries oxygen and gives blood its red colour.
The sickle cell genes make the body produce unusual haemoglobin called HbS. (Normal haemoglobin is called HbA.) HbS behaves in a different way from HbA. Under certain conditions, HbS makes the red blood cells change shape – instead of the typical doughnut shape, they become sickle-shaped, like a crescent moon. This is called sickling. Conditions which trigger sickling are cold, infection, lack of fluid in the body (dehydration), low oxygen, and acid (acid is produced in hard exercise).
How is Sickle Cell Disease Diagnosed?
The diagnosis is made by a blood test. The blood sample is analysed to see what type of haemoglobin exists in the blood (using a test called haemoglobin electrophoresis or other methods).
In England, Scotland and Wales, there is a screening program to test pregnant women and newborns for SCD and other haemoglobin disorders. Northern Ireland currently checks newborns as part of the bloodspot test but not pregnant women.
What are the Symptoms of Sickle Cell Disease?
Symptoms of SCD come and go. Usually there are bouts (episodes) of symptoms however, between episodes, you feel well. The factor that symptoms reoccur is that the red blood cells can act generally for much of the time – but if something makes too many of them sickle, the sickle cells cause symptoms. If there are severe and sudden symptoms due to sickling, this is called a sickle cell crisis.
There is a great deal of specific variation in symptoms – how many and how often you get them. Some individuals with SCD have frequent symptoms, while others have few and their sickle cell disease is barely obvious. For the majority of people, symptoms are somewhere between these two extremes. The majority of people with SCD have a few episodes of sickle cell crisis each year.
Symptoms usually start after a few months of age. (Before that age, the baby has a different haemoglobin, called fetal haemoglobin, which is not affected by the sickle cell gene).
The various symptoms that can happen if you have SCD include:
Episodes of pain
These are likewise called a pain crisis or a vaso-occlusive crisis. They happen when sickle cells obstruct small capillary in bones, which causes pain. Pain typically occurs in bones and joints. The pain can vary from mild to severe, and might begin suddenly.
A common symptom in children and young children is when small bones in the fingers and toes end up being swollen and painful – this is referred to as dactylitis.
Episodes of tummy (abdominal) pain can occur if sickle cells block capillary in your abdominal area.
Acute chest syndrome
This happens when there are obstructed capillary in the lungs and can in some cases occur with a lung infection.
The symptoms can include chest pain, high temperature level (fever) and shortness of breath. Children and children might have more vague symptoms and look usually weak, be lacking in energy (sluggish), be restless or have quick breathing. Acute chest syndrome is really serious and, if it is presumed, you need to be treated urgently in health center.
Intense chest syndrome can begin a few days after a painful sickle crisis. It is most common in women who are pregnant or who have just recently had a baby.
Infections
Individuals with SCD are more susceptible to severe infections, especially from certain types of germs (bacteria), which can cause pneumonia, meningitis, septicaemia or bone infections. (These include the pneumococcal, Haemophilus influenzae type b and meningococcal bacteria, and salmonella bacteria which can infect bones).
Symptoms of infection include fever, feeling normally ill, and pain in the affected part of the body.
Children with SCD have a high risk of getting severe or lethal infections. It is very important to see a doctor quickly if you think an infection or feel unhealthy.
Keep in mind: a fever can occur in a sickle cell crisis without having an infection.
Anaemia episodes
Anaemia is a lack of haemoglobin in the blood. As pointed out above, individuals with SCD will generally have a moderate anaemia, which does not typically cause problems. Nevertheless, sometimes, individuals with SCD can get a severe anaemia, which can be serious. It may come on extremely unexpectedly or more gradually. Immediate treatment may be required.
Symptoms of severe anaemia are:
- Feeling exhausted, faint, short of breath, dizziness, feeling ill (nausea) or having quick breathing – worse with exercise.
- Children and kids might be lethargic, not feeding much or typically unwell.
- A pale skin colour (easiest to see in the lips, tongue, fingernails or eyelids).
- With children, the spleen in some cases enlarges rapidly and causes unexpected severe anaemia. The enlarged spleen is in the abdomen and can be felt. Parents might be shown how to feel their child’s spleen. If the spleen enlarges quickly, it is a sign that immediate treatment is needed.
What is the Treatment for Sickle Cell Disease?
In most cases, SCD can not be cured, so long-lasting treatment and monitoring are required. There are a number of various treatments which help to prevent sickling episodes, or avoid associated problems such as infection.
Principles of Treatment
- You need to be treated by an expert doctor or team, experienced in treating patients with SCD. If the specialist is a long way from your home then a few of your treatment might be with a more regional hospital or doctor – however the local physicians need to get recommendations from your professional.
- Due to the fact that symptoms of SCD can begin unexpectedly, you need to have the ability to see a doctor and get hospital treatment urgently, as and when needed.
- You can be demonstrated how to identify symptoms (in yourself or your child), so that treatment can be begun quickly.
- Treatment must be customized to your specific requirements.
- It is essential to take preventative treatments against infection, and to attend your check-ups.
Stem cell transplant is the only available treatment that can treat SCD. It is just used for severe SCD. Its use is restricted by side-effects of the procedure and the availability of appropriate donors.
Home Treatment for Sickle Cell Disease
Home treatment for sickle cell disease consists of actions to manage pain and avoid complications of the disease. If you don’t already have a home treatment plan, ask your doctor to assist you make one. Use this plan whenever symptoms are present. Your plan might include suggestions for:
- Managing pain.
- Home treatment for prolonged erection of the penis (priapism).
- Staying healthy.
- Handling stress and concern.
Managing a child’s unique requirements
You can help your child deal with special requirements in school by:
- Making plans with instructors or a tutor to assist your child equal schoolmates when disease causes absences from school.
- Explaining to teachers that children with sickle cell disease may have to use the restroom regularly than other kids. They also require more water than the other trainees. Not consuming sufficient water can raise the opportunity of a sickle cell crisis.
- Educating instructors and other school staff members about the signs and symptoms of sickle cell disease that require immediate healthcare. Composed instructions will help school personnel understand what to do and who to contact an emergency situation.
Children with sickle cell disease can typically work out and play typically if they:
- Drink plenty of fluids before, during, and after workout. Absence of fluids (dehydration) can cause cells to sickle.
- Get regular rest breaks during energetic workout.
- Stay warm. Direct exposure to cold air, wind, and water can activate a sickle cell crisis. Gown children in warm layers of clothing for cold-weather experiences. Your child should prevent swimming and playing in cold water.
Folic acid supplements are often a necessary part of the diet for people with sickle cell disease, especially if you aren’t eating enough folate-rich leafy veggies (such as spinach).