Fungal skin diseases (mycoses) are pathologies that people encounter regularly. Such lesions take first place among all diseases of infectious nature. Such prevalence of pathology is due to the fact that not everyone knows how to prevent mycoses and what to do if they occur.
In fact, you should just go to the doctor in a timely manner and prevent the development of neglected forms of fungal diseases. In the early stages of all fungal infections are successfully and quickly enough treated. Today there are tested methods, which allow you to eliminate both the external symptoms of the pathology and the causes that provoke its development. Don’t be ashamed of your problem!
Causes of fungal skin infections
Fungal diseases are contagious. Their main cause is the transmission of the pathogen by wearing the same shoes, using other people’s towels, walking barefoot in public places (especially with high humidity): saunas, baths and swimming pools. Fungal infections can be transmitted by direct contact with an infected person, plant or animal.
Risk factors include:
- Traumatic skin injuries
- Weakened immunity
- Prolonged treatment with antibiotics
- Avitaminosis
- Chemotherapy
- Excessive sweating
- Overwork
- Chronic diseases of the nervous system and other systems
- Failure to follow hygiene rules
- Skin contact with aggressive chemicals
- Occupation associated with staying in toxic environments, conditions with high humidity, etc.
As a rule, infection occurs in:
- Gyms
- Swimming pools, saunas and baths
- Massage rooms
- Manicure salons
- Hairdressing salons
- Beauty salons, etc.
You can catch skin fungus infections in hotels or on the beach, even at home if you don’t keep your apartment clean and tidy.
Important! Do not be ashamed of the problem. Anyone can catch “fungus”, even people who try to follow hygiene. Pathogenic flora is everywhere and can instantly penetrate into the body (especially if your immune system is weakened – a recent illness, for example).
Symptoms
Symptoms of fungal skin infections appear the same in adults and children. It is not age that determines the symptoms, but the affected area.
Pathogens can multiply on the skin (any part of it) and mucous membranes.
The classic symptoms for all fungal diseases are:
- Burning sensation
- Itching (both mild and intense)
- Color changes in the affected area
- Flaking of the skin
In mycosis of the feet on the surface of the skin:
- Variously shaped spots with altered coloration appear
- Desquamation occurs
- An inflammatory process is provoked, accompanied by a local rise in temperature
Some patients complain of an unpleasant smell, blisters in the folds of the fingers, which are itchy and deliver discomfort.
With mycosis on the face, the main symptoms are:
- Patches with altered coloration
- Skin flaking
- Coarsening of the skin
Usually at the initial stage, fungal diseases do not manifest themselves in any way, because only dead epidermal cells are affected. But if you do not start treatment in time, mycosis will deliver a lot of problems.
Over time:
- The spots on the face will enlarge and spoil the appearance
- Ulcers, cracks and pus-filled lesions will develop
- The face will become increasingly itchy
Facial fungus often causes the patient a lot of complexes. Some people with advanced stages of the disease even refuse to go out, because they are embarrassed of their appearance.
With mycosis on the scalp, patients complain about:
- The appearance of pink plaques.
- Deterioration of hair, hair loss, and even the appearance of bald spots
- Peeling
- Hair brittleness at the base
Symptoms of fungal diseases also depend on the type of lesion.
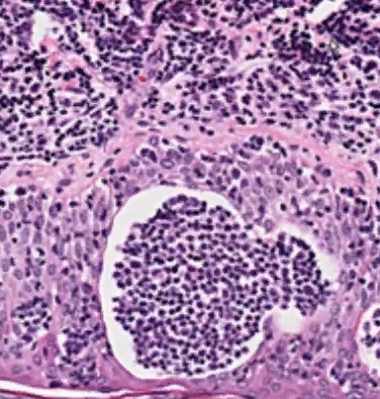
With dermatomycosis there is a deep lesion of the skin with mold or yeast fungi. Such pathology stimulates the development of an inflammatory process and is usually accompanied by the appearance of spots of different sizes with pink and red coloration.
In keratomycosis, the fungus affects the upper layer of the skin. The inflammatory process may be absent. Small nodules with purulent contents usually form on the skin.
Candidiasis affects the mucous membranes. Usually, spots form in the armpits, under the mammary glands (in women), as well as in the groin area.
With deep mycosis, the subcutaneous tissue is affected. Also, the pathological process affects the mucous membranes and even the internal organs and nervous system. The skin is covered with unsightly warts and fistulas with purulent contents.
At any sign of fungal skin infection you need to see a doctor as soon as possible. Treatment for fungal skin diseases of the face, body, nails will be prescribed immediately after all symptoms are detected and diagnosed.
Diagnostic methods
As part of the diagnosis of mycoses, scrapings of skin and nails, sputum, blood, hair, mucous membrane scrapings, feces and other biomaterials may be examined, depending on the type and localization of the lesion. In case of skin diseases, it is usually performed:
- Dermatoscopy – examination of affected areas of skin, hair or nails to identify characteristic signs;
- Microscopic examination of a scrape to detect fungal mycelium;
- bacterial culture on nutrient media, which reveals not only the type of fungus, but also the optimal drug for treatment;
- serological blood test;
- PCR test to detect the fungus genome.
- Some types of fungi are quite easily diagnosed with the help of UV light, which is generated using a Wood lamp.
Simultaneously with determining the type of fungus, the patient undergoes a general examination to determine the cause of the weakened immunity that led to the infection.
Treatment of fungal skin infections
Treatment of fungal diseases of the nails, scalp, mucous membranes and skin is a complex and long process. This is primarily due to the fact that the pathology often occurs against a background of weakened immunity. Nevertheless, therapy is successful with a comprehensive professional approach.
Treatment of fungal skin diseases of the hands, feet, face, head and nails is always carried out using a whole complex of drugs and techniques. Both tried and tested means and new antimicrobial preparations are used. Compounds that completely kill the infection and prevent it from spreading are also used.
The treatment program depends a great deal on:
- The diagnosed disease
- The patient’s state of health (including the presence of concomitant diseases)
- The stage of the infectious process
Comprehensive treatment of fungal diseases of the nails, skin and mucous membranes includes:
- Prescription of local and systemic agents
- Therapy of the underlying pathology, against which the infection occurred
- Vitamin therapy, etc.
The treatment of the patient’s belongings is mandatory. Some items of personal use (towels, for example) will have to be replaced by new ones, as it is almost impossible to clean them properly at home. It is very important not only to take all the prescribed medications, but also to carefully observe all the rules of personal hygiene.
Topical treatment for fungal skin diseases
Medicinal products for topical use are made in the form of lotions, ointments, drops, sprays and even nail polish. Using them is simple enough, but it is important to always follow the exact dosage and focus on the recommendations issued by the doctor. As a rule, remedies are applied to the affected areas. Local treatment allows you to eliminate the symptoms of the disease quickly enough.
Today, the following drugs are actively used:
- Antimycotic medicines with antibiotics and corticosteroids. Such drugs are prescribed for damage to the skin and mucous membranes, swelling. They are effective for both primary and secondary infection
- Drugs that kill the fungal infection and prevent its further spread. These drugs are prescribed only when the inflammatory process subsides (if it developed)
- Remedies to eliminate itching
- Moisturizing and nourishing preparations for the skin. Such means are used during rehabilitation and allow the skin to recover, saturating it with moisture and all necessary nutrients.
How do medications for the treatment of fungal skin infections work?
Dermatologists and mycologists practice a comprehensive, step-by-step approach to the treatment of fungal skin lesions – mycoses. It is aimed at destroying infectious agents and eliminating the symptoms of an extremely infectious disease.
And also to strengthen local immunity, which becomes an excellent prevention of re-infiltration of fungi into the skin. For this purpose, doctors usually prescribe patients external remedies – ointments, creams, gels, solutions, lotions.
To treat skin mycoses, effective preparations with fungicidal action are used. The active substances block squalene-2,3-epoxidase, an enzyme that triggers the production of ergosterols needed by fungi to build membranes. As a result, cell permeability increases. Intercellular fluid with dissolved macro- and microelements easily penetrates into them. The cell undergoes lysis (dissolution) and is destroyed from the inside.
Which drugs are fungicides:
- Nizoral;
- Exoderil;
- Terbinafine;
- Mycosyst;
- Mycoderil;
- Batrafen;
- Lamisil;
- Fungoterbin and others.
There is also a group of drugs with fungistatic activity. Their components are not capable of destroying pathogens. They create an environment very unfavorable for their growth and reproduction. After the use of drugs, the spread of the infectious and inflammatory process slows down, but it does not go anywhere.
For foot fungus
Foot fungus leads in the ranking of mycoses of the skin by the number of detected cases. According to some data, it is diagnosed in 15-20% of the world’s population.
And this despite the annual arrival of modern drugs on the pharmaceutical market, as well as tools for prevention. Pathogens quickly lose sensitivity to them, so even prolonged treatment does not bring results.
The list of ointments, to the components of which the fungal cells are not yet resistant:
- Lamisil;
- Terbinafin;
- Clotrimazole;
- Microsporum;
- Exoderil;
- Bifosin;
- Exifin;
- Mykonorm.
After the infectious agents have died, the skin condition immediately improves. The skin ceases to itch and inflame, and the pain that worsens when you walk disappears. The use of these remedies prevents fungi from penetrating the nail plates. Use them together with antiseptic solutions – Furacilin, Chlorhexidine.
For hand fungus
Mycosis is localized on the hands, usually between the fingers. The skin there is the most delicate, thin, sensitive skin, so you need effective, but the safest ointments and creams. After all, if it becomes too dry, the problem only gets worse – fungi and pathogenic bacteria invade the microcracks.
The mildest, gentlest action has the following preparations:
- Candide;
- Imazole;
- Canesten;
- Mycosolone;
- Zalain;
- Myconazole;
- Onabet.
Ointments help prevent maceration – the dissolution of the intercellular substance. At the same time, they dry out well, reduce irritation and eliminate small rashes. They can also be applied to elbows, wrists, forearms and armpits.
For the body
Signs of fungus on the body are pink-red ring-shaped spots with slightly raised flaky edges. If a person does not immediately go to the doctor, practicing self-treatment, it does not take long to wait for complications. Staphylococcal or streptococcal bacterial infection joins fungal.
To prevent negative developments, it is necessary to immediately apply ointments with a powerful fungicidal effect:
- Nystatin;
- Terbinafine.
- Mycoseptin;
- Zalain;
- Ketoconazole;
- Lamisil;
- Nitrofungin;
- Mycosolone.
In skin folds, including groin folds, Candida yeast-like fungi, aka the causative agents of candidiasis, “settle”. An interesting fact is that they are perfectly coped with a drug synthesized many decades ago. It is a cheap antimycotic Clotrimazole, which you can buy in any pharmacy.
For genital areas
Fungi affecting male and female genitals are always there. They should not be confused with venereal infections. Although they can be transmitted through sexual contact. The trigger for their increased activity is usually a weakening of the immune system due to a sudden exacerbation of a chronic disease or a developed violent allergic reaction. Doctors prefer to treat vaginal fungus with both ointments and vaginal suppositories, balls, and pills.
Any drug that contains the following active ingredients will help:
- miconazole;
- clotrimazole;
- isoconazole;
- natamycin.
And for men is designed cream Pimafucin. Even after a single treatment of the skin on the inner surface of the thighs, most of the infectious agents are killed.
Nystatin-based products have recently become less and less common in the treatment of inguinal candidiasis. It was found that the ointments destroy not only pathogens, but also lactobacilli living in the vagina. And they are the body’s natural defense against fungi, viruses and bacteria. If your doctor has prescribed nystatin, use it, but then take a course of probiotics (Linex, Acipol, Hilac Forte) for 7-10 days to restore vaginal microflora.
For children
Newborns, too, are not immune to mycosis pathogens. Fungi are transmitted to them from the mother when they pass through the birth canal or in the first months of nursing. They can penetrate the skin with diaper rash or damaged by diaper dermatitis. Because babies’ immune systems are in their formative stages, the safest possible antimycotic agents are needed.
The most effective of these are:
- Clotrimazole quickly destroys the cells of pathogenic and conditionally pathogenic fungi, prevents the attachment of bacterial infection;
- Mycoseptin (from 2 years) has a pronounced fungicidal effect, cleanses the dermis and epidermis of pathogens;
- Pimafucin shows activity against a variety of fungi – yeast-like, yeast, dermatophytes.
Often doctors do not prescribe antifungal agents to young patients, even if the list of contraindications does not include age restrictions. For example, the use of Exoderil in the annotation is not prohibited. But at the same time, it is indicated that no clinical trials have been conducted, the results of which would confirm the safety of the drug for this group of patients. Do not hesitate to ask your doctor a question about it. It is quite possible that he will go to a meeting, and choose another antifungal agent for the child.
Systemic treatment of fungal diseases
Systemic medicines are available in the form of tablets, capsules and solutions for injection. Usually these drugs are prescribed in the middle and severe stages of the disease. This is due to the fact that in such situations, only relieving symptoms is not enough. The infection has already had an impact on the internal organs and body systems.
Usually prescribed:
- Azoles. Such drugs stop the growth and reproduction of fungi, causing their death
- Allilamines. Such drugs prevent the development of fungi.
- Important: Do not self-treat fungal diseases of the face, hands, feet and other parts of the body. The dosage of all drugs and the time of their use should be determined only by a specialist.
You should also understand the high risks that the therapy will not be effective.
The main reasons for the decrease in the effectiveness of treatment include:
- Violation of hygiene rules by the patient. Some people do not take the detected pathology seriously enough. They think that fungal infections are not dangerous and do not require systemic and comprehensive therapy. If during even the most intensive treatment constantly contact with the source of infection, there will be no effect
- Self-treatment. Some patients, on the contrary, are very afraid of the spread of fungus. They want all symptoms to disappear in just a few days, and it seems that the doctor has prescribed an insufficient amount of drugs. Additional drugs are independently included in the complex of therapy. Often they not only do not give the desired effect, but also aggravate the situation.
- Refusal of treatment after it has begun. Patients who do not see the effect in the first few days believe that the therapy is ineffective, and abandon it. Of course, this leads to the fact that the fungus actively multiplies further, and the symptoms worsen
If you want the treatment to be effective, take all the prescribed drugs, follow the rules of hygiene and regularly visit the doctor to diagnose the condition. This will quickly get rid of the symptoms and causes of the pathological process.
Interview with a dermatologist about fungal skin infections
Television and the Internet offer various medications for toenail fungus. What kind of disease is this?
Fungal infection, or mycosis of the feet, is one of the most common diseases of the feet, nails and interdigital space. According to official statistics, 35% of the population suffers from this infection today. However, not all patients may immediately realize that they are developing foot mycosis, so they are in no hurry to see a doctor. They come when the problem becomes noticeable. This, of course, complicates and increases the period of treatment, the concentration of the influencing substance on the fungus also increases.
How can a person understand that he has contracted foot mycosis?
One of the first symptoms is redness, a feeling of itching and burning of the skin of the feet, cracks in the skin between the toes. It is worth paying attention to the nails: the thickness of the nail plate, its color, structure changes; the nails become thickened or brittle, crumbling; the skin around the nails becomes red, swelling of the perenal fold. A peculiar odor may appear. If the patient has even the slightest suspicion of a mycological infection, it is necessary to go to a medical facility to a dermatologist or mycologist.
But why does it happen? Where and how?
In the risk area – public places, water complexes sports facilities, especially locker rooms, steam rooms, baths, the beach. I want to remind you that you can’t wear other people’s shoes, walk barefoot in public places. Do not forget about the disinfection of manicure equipment. Unfortunately, a fungal infection can lead to excessive sweating, reduced immunity, endocrine disorders, chronic diseases, as well as diabetes, hypo-and avitominosis, obesity, HIV.
We would like to draw the attention of pet owners: the summer cottage season is coming, so do not forget to inspect your pets. If you find a hole in the hair, changes in fur, redness of skin of your pet, you should go to the veterinarian.
Fungal infection used to be not talked about so often, but now everyone knows about this disease. Are there more people getting sick?
There is no more infection, there is more public awareness. And forewarned is forearmed.
Of course, bad nails look unattractive, to say the least, but what harm does fungal infection do to the body?
Onychomycosis can lead to other diseases – such as bronchial asthma, various skin diseases of allergic etiology.
The nail polishes that are advertised on TV can really cure nails? Or can’t you do without a doctor’s help?
Only a doctor can prescribe a treatment. Altered nail plates do not always indicate a fungal lesion of the nails. Thus, nail plate lesions are found in onychodystrophy, hypo- and avitaminosis, anemia, psoriasis, traumatic lesions and other pathologies.
There are also folk remedies, which, as they say, grandmother prescribed. Is it possible to heal with their help on your own?
I would not listen to this advice. A patient who goes to the branches of the Moscow Scientific and Practical Center for Dermatovenerology and Cosmetology of the Department of Health of Moscow will necessarily conduct a laboratory study on the type of causative agent of mycological infection, and if necessary, a study on the sensitivity of the infectious agent to antimycotic drugs.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.