Anal fissures are a common problem often faced by people all over the world. And despite the fact that it is a rather sensitive topic, it should be addressed for everyone’s benefit. Nevertheless, a thorough understanding of anal fissures is essential for choosing appropriate treatments.
Understanding Anal Fissures
An anal fissure is a small tear or cut that occurs in the lining of the anus. While it can impact people of all ages, it is more prevalent in young adults and children. These painful tears can be caused by multiple factors including passing hard or large stools, dealing with chronic constipation, experiencing persistent diarrhea, or even as a result of trauma from anal intercourse (Intercourse in the anus is a great sin whether you do it with your wife or not!)
Causes
An anal fissure is a small tear in the lining of the anus, which can cause significant pain and bleeding during and following bowel movements. Below is a chart outlining common causes, their reasons, and tips on how to avoid them:
| Cause | Reasons for the Cause | How to Avoid the Cause |
|---|---|---|
| Hard Stools or Constipation | Passing large or hard stools can tear the anal lining. | Increase fiber intake, stay hydrated, and exercise regularly to promote healthy bowel movements. 🥗💧🏃♂️ |
| Childbirth | The strain of giving birth can cause stretching and tearing of the anal canal. | Perform pelvic floor exercises and follow medical advice during pregnancy and delivery. 🤰🏋️♀️ |
| Diarrhea | Chronic diarrhea can irritate the anal area. | Treat underlying conditions and consume a balanced diet to maintain solid bowel movements. 🚫🌶️ |
| Anal Intercourse | Physical trauma from anal intercourse can lead to fissures. | Use lubrication and practice safe, gentle techniques. 🛑✨ |
| Crohn’s Disease or IBD | Inflammatory bowel diseases can cause inflammation of the anus. | Work with a healthcare provider to manage IBD effectively. 💊 |
| Decreased Blood Flow | Aging or other factors might decrease blood flow to the anal area. | Maintain general cardiovascular health through diet and exercise. 🚴♂️❤️ |
| Anal Cancer or Infections | These can lead to abnormal changes in the anal tissue. | Regular medical check-ups and prompt treatment of infections. 🏥🩺 |
It’s essential to note that while some causes of anal fissures can be mitigated through lifestyle changes, not all are avoidable, such as those related to underlying medical conditions. In such cases, consistent medical care is critical.
Symptoms
Symptoms of anal fissures may differ among individuals, though several commonly observed indications are:
- People with anal fissures often feel severe pain while having bowel movements and also afterwards.
- The presence of bright red blood may be observed either on the toilet paper or in the toilet bowl after having a bowel movement.
- Pruritus: The sensation of itching around the anus may be experienced as a result of the irritation caused by the fissure.
- Sensitivity and a gentle touch can cause discomfort in the affected area.
- Anal sphincter spasms, also referred to as involuntary contractions of the anal muscles, can be experienced by certain people.
If you consistently observe these symptoms or encounter intense discomfort, it is crucial to seek medical advice from a healthcare expert to receive an accurate diagnosis.
Treatment Options
The treatment for anal fissures depends on the severity and duration of symptoms. The following are some commonly used treatment options:
- Modifications to one’s lifestyle and diet can be made to improve digestive health. These adjustments involve consuming more fiber, staying hydrated, and refraining from straining when using the bathroom. These changes work towards softening the stools, making them easier to excrete and relieving pressure on the anus.
- Topical medications refer to creams or ointments that do not require a prescription and contain components such as hydrocortisone or lidocaine. These can be utilized for easing pain, diminishing inflammation, and aiding in the healing process.
- Stool softeners and bulk forming agents may be recommended by a medical professional to promote regular and easier defecation, thus reducing the likelihood of additional irritation to the fissure.
- Nitroglycerin cream may be recommended by doctors in certain situations to help relax the muscles of the anal sphincter, promoting healing and providing pain relief.
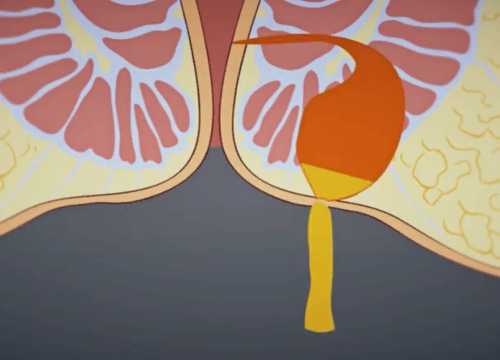
- If conservative treatments fail to provide sufficient relief, doctors may suggest surgery as an option. Surgical procedures for this condition include sphincterotomy, where a small section of the anal sphincter muscle is cut to alleviate pressure, or lateral internal sphincterotomy, which involves cutting the internal sphincter muscle.
Remembering that each case is one-of-a-kind, it is essential to seek advice from a medical expert to establish the most suitable course of treatment.
Preventing Anal Fissures
Prevention is always better than cure. To minimize the risk of developing anal fissures, consider adopting the following measures:
- To keep your digestive system healthy and avoid constipation, it is important to include a lot of fiber in your diet. Adding fiber-rich foods to your meals, like fruits, vegetables, whole grains, and legumes, can help regulate your bowel movements.
- It is important to stay well-hydrated as drinking enough water can assist in keeping stools soft, therefore making them easier to expel.
- In order to prevent infection and additional irritation, it is important to practice good hygiene by gently cleaning the anal area with mild soap and water after having a bowel movement.
- To prevent the occurrence of fissures, it is advisable to refrain from exerting excessive force when passing stool. Applying too much pressure in the anal region can elevate the chances of developing cracks. Instead, it is important to maintain a relaxed state and take sufficient time while using the toilet.
Conclusion
Being knowledgeable about the symptoms, causes, and treatment options for anal fissures can greatly assist individuals in dealing with the discomfort they cause. Seeking medical assistance promptly and taking preventive measures can play a crucial role in managing and preventing anal fissures, ultimately leading to a healthier and more satisfying life. It is important to remember that open communication with a healthcare provider is crucial in addressing concerns and receiving the proper care.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.