You’re sitting in the bathroom, minding your business, when suddenly—green poop? It’s a moment that makes you blink twice. Is your digestive system staging a rebellion? Or did that kale smoothie really go the extra mile? Before you spiral into a WebMD rabbit hole, let’s unpack this peculiar yet common occurrence and understand what your stool is trying to tell you.
Age Groups Most Likely to Report Green Stool
This chart displays the percentage of people in each age group reporting green stool symptoms. The values are visually scaled up threefold to emphasize differences between age categories more clearly.
Why Does Poop Turn Green?
Poop gets its color from a mix of bile and the byproducts of digested food. Bile, which is produced in the liver and stored in the gallbladder, starts off as a greenish fluid. As it moves through the intestines, enzymes and bacteria usually break it down and change its color to the familiar brown. When this process is rushed—say, because of diarrhea or a hyperactive digestive system—the bile doesn’t get fully processed and stays green, coloring your stool.
Think of it like overcooking spinach: if you don’t give it time to break down, it retains its strong green pigment. Similarly, bile needs time to chemically transform. If your gut is moving like a bullet train, there’s simply no chance for that color change to happen.
This can happen to anyone, but it’s particularly common in people with fast digestive transit, including children, those with gastrointestinal infections, or individuals with irritable bowel syndrome (IBS). Even athletes or people who recently changed their diet drastically—especially with high-fiber or detox foods—might notice green poop.
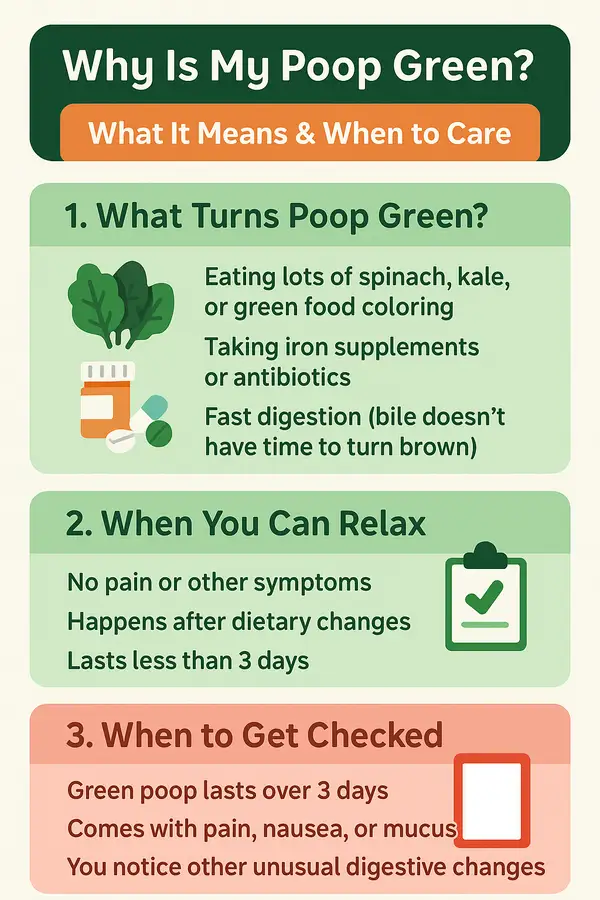
Common Causes of Green Poop
Dietary Habits
Green leafy vegetables like kale and spinach, or food coloring in cereals and candies, are common culprits. Fun fact: indulging in vibrant green smoothies might make you feel healthier, but they can also give you a colorful surprise! source
Dietary Triggers of Green Poop
This chart visualizes the frequency of green stool associated with different dietary sources. Values have been doubled to better highlight the proportional influence of each trigger.
Supplements and Medications
Iron supplements and certain antibiotics can also turn your poop green. If you’re popping those iron pills like candy, this might be your answer. source
Digestive Speed
When digestion moves quickly, bile doesn’t get processed fully, leading to green stool. Conditions like diarrhea or irritable bowel syndrome (IBS) are prime examples of this speedy process. source
When Should You See a Doctor?
While green poop is usually harmless, certain situations warrant medical attention:
- Persistent green stools lasting more than a few days.
- Accompanied by severe abdominal pain, nausea, or vomiting.
- Presence of mucus, blood, or other alarming symptoms.
In such cases, consulting a healthcare professional is crucial. source
Diagnosing the Underlying Cause
Doctors typically start with a comprehensive history and physical exam. Here are common diagnostic tools used:
| Diagnostic Method | Procedure & Details | Accuracy (1-10) | Avg. Cost (USD) |
|---|---|---|---|
| Stool Analysis | Sample analyzed for bacteria, parasites, or blood | 8 | $100-250 |
| Blood Tests | Assess liver function, infections | 9 | $150-300 |
| Colonoscopy | Detailed colon examination using a camera | 10 | $1000-3000 |
Technologies like capsule endoscopy, a pill-sized camera that captures images inside your digestive tract, have also emerged as innovative diagnostic tools, offering detailed insights without invasive procedures. source
Real-Life Medical Case
Consider this interesting medical case from Austin, Texas: A 32-year-old man visited his doctor after noticing green stool for nearly a week. Surprisingly, his love for spirulina smoothies turned out to be the cause. Once he adjusted his diet, his poop returned to its normal brown hue, leaving him both relieved and slightly amused. source
Treating Green Poop
Most cases of green poop don’t require invasive procedures and typically resolve quickly with lifestyle and dietary adjustments. For example, stopping iron supplements or reducing intake of green-colored foods can lead to improvement within a few days.
When medications are necessary, probiotics like Align or Culturelle may help restore healthy gut flora, improving digestion within one to two weeks. These generally cost around $20 to $50 for a month’s supply.
If diarrhea or IBS symptoms persist, anti-diarrheal medications like Imodium (loperamide) may be recommended. They provide rapid relief within hours, but their long-term effectiveness is limited without addressing the root cause. Costs are usually between $10 to $25.
Treatment Choices for Green Poop Relief
This chart represents the most common initial treatments selected by patients for green stool relief. The data is doubled in scale to better emphasize the preference distribution.
In rare instances where inflammation or infection is identified, prescription antispasmodics or antibiotics may be prescribed. These are highly effective (rated around 9 on effectiveness), with noticeable symptom relief typically within 24 to 72 hours. However, they require physician supervision and cost around $50 to $200 depending on medication type and duration.
Editorial Advice
Green poop typically isn’t something to lose sleep over. However, as Reyus Mammadli, medical consultant, recommends, “Never hesitate to consult a healthcare provider if symptoms persist, as it could indicate an underlying condition needing attention.”
Remember, occasional green stool is generally as harmless as finding a dollar bill on the sidewalk—a little surprising but usually nothing to worry about. Keep an eye on persistent or worsening symptoms, and when in doubt, it’s always wise to get a professional opinion. source
FAQ: More Insights on Green Poop
1. Can stress or anxiety cause green poop?
Yes, stress and anxiety can impact your digestive system and speed up intestinal transit time. This means bile has less time to break down, potentially leading to green stools. While this isn’t harmful in itself, if green poop coincides with ongoing anxiety symptoms, it might be worth addressing both issues with a professional. Managing stress with behavioral techniques and ensuring a fiber-rich diet can help normalize stool color.
2. Does green poop indicate a parasite infection?
Sometimes, yes. Parasites like Giardia can cause changes in stool color, including green hues, especially when accompanied by diarrhea or greasy texture. These infections often come from contaminated water or undercooked food. Diagnosis requires a stool sample and treatment typically involves prescription antiparasitics like metronidazole. If you’ve traveled recently or consumed questionable water, testing is essential.
3. Is green poop during pregnancy a cause for concern?
In most cases, no. Hormonal shifts, prenatal vitamins (especially those with iron), and dietary changes during pregnancy can lead to green stool. As long as there are no other symptoms like pain or bleeding, green poop is generally harmless. However, if accompanied by severe gastrointestinal distress, a prenatal healthcare provider should evaluate it.
4. How does intermittent fasting affect stool color?
Intermittent fasting can lead to green poop by altering digestion speed and bile processing. When you eat after a long fast, your digestive system may move food more quickly, giving bile less time to change color. Additionally, high intake of leafy greens or supplements during eating windows can influence this. It’s not harmful unless persistent or paired with discomfort.
5. Can dehydration play a role in green poop?
Yes, although indirectly. Dehydration can lead to concentrated bile and sluggish digestion in some people, but in others, it may contribute to diarrhea, especially if paired with caffeine or sugar. This quick movement through the gut leaves bile green. Keeping hydrated helps maintain balanced digestion and healthy bowel movements.
6. What role does liver function play in stool color?
The liver produces bile, so its health directly impacts stool color. If bile production or flow is compromised—due to conditions like hepatitis or gallstones—stools may appear pale, yellow, or even green. Consistent green or pale stools, especially with fatigue or jaundice, should prompt liver function tests. Early diagnosis is crucial for managing liver-related conditions.
7. How do artificial sweeteners affect bowel color?
Certain sugar substitutes like sorbitol or sucralose can speed up gut motility, leading to looser or green-tinted stools. They’re often found in diet sodas, sugar-free gum, and protein bars. Not everyone reacts the same way, but excessive intake may trigger digestive changes. Reducing or eliminating these can resolve unusual stool colors.
8. Could green poop be a symptom of celiac disease?
It’s possible. Celiac disease can cause malabsorption and rapid transit time, which may result in green stools—especially during flare-ups or undiagnosed stages. Additional symptoms include bloating, fatigue, and weight loss. A blood test for tTG-IgA followed by a biopsy confirms the diagnosis, and treatment involves a strict gluten-free diet.
9. Are there any chronic conditions linked to green poop?
Yes, inflammatory bowel diseases like Crohn’s or ulcerative colitis can cause green stool, particularly during flare-ups. These conditions affect how the intestines absorb nutrients and handle bile. Persistent green stool along with abdominal pain, fatigue, or rectal bleeding may indicate a chronic gastrointestinal disorder. A gastroenterologist should evaluate these symptoms for proper diagnosis and treatment.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.







