Bloating and abdominal pain are among the top complaints in both primary care and gastroenterology offices across the United States. It’s a frustrating and sometimes embarrassing condition that affects millions of Americans every year. In fact, up to 30% of adults report experiencing bloating regularly, with women twice as likely to suffer from it as men. So what’s going on down there?
Source: iythealth.com
At its core, bloating is a feeling of fullness or swelling in the abdomen, often accompanied by pain, discomfort, or visible distention. It can result from a wide range of causes—from the innocent (like overeating) to the more serious (such as gastrointestinal diseases). Understanding these triggers is crucial not only for relief but also for preventing future flare-ups.
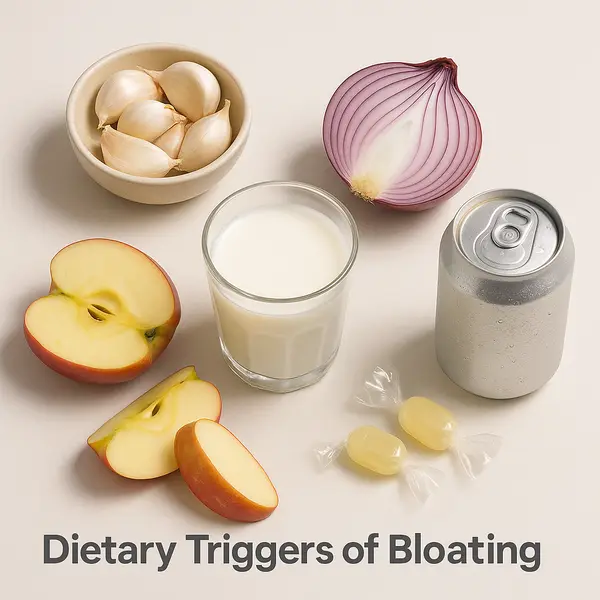
Common Dietary Triggers That Can Wreck Your Gut
You are what you eat—and sometimes, what you eat fights back. Certain foods are notorious for causing bloating and gas. Here are the biggest dietary offenders:
- High-FODMAP foods: FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) are short-chain carbohydrates that are poorly absorbed in the small intestine. Foods high in FODMAPs include garlic, onions, apples, and wheat. When fermented in the gut, they produce gas and draw water into the intestines. Think of them as the party crashers of your gut—they show up, cause a commotion, and leave your belly gassy and swollen.
- Carbonated beverages: That fizzy soda or sparkling water might feel refreshing but can introduce excess air into your digestive system, causing belching and bloating. It’s like blowing up a balloon inside your stomach—eventually, all that trapped gas wants out, one way or another.
- Artificial sweeteners: Sorbitol and mannitol, commonly found in sugar-free products, are poorly absorbed and can ferment in the colon. These sugar substitutes sneak past your small intestine undigested and become buffet material for bacteria in your colon—cue the gas and bloating.
- Dairy: Lactose intolerance is a common culprit, particularly in Hispanic, African American, and Asian American populations. When lactose isn’t digested, it becomes fuel for gut bacteria, which leads to gas and discomfort. Imagine pouring milk into a system that doesn’t have the tools to break it down—it’s like trying to wash dishes without soap: messy, inefficient, and full of residue.
In a recent study published by the American Journal of Gastroenterology, nearly 75% of participants who followed a low-FODMAP diet reported significant improvement in bloating ⧉.
Weekly Bloating Prevalence by Age Group
This chart shows how frequently people in different age groups experience bloating at least once per week. The trend indicates that younger adults report bloating more often, with prevalence gradually decreasing with age. Global studies suggest that around 18% of adults overall experience weekly bloating, with lower rates observed in older populations.
Medical Conditions That Might Be to Blame
Sometimes, bloating isn’t just a food issue. Several underlying medical conditions can cause both bloating and abdominal pain:
- Irritable Bowel Syndrome (IBS): IBS affects up to 15% of Americans and is a leading cause of chronic bloating. It’s often accompanied by cramping, diarrhea, or constipation. Think of IBS like a traffic jam in your intestines—things move too quickly, too slowly, or erratically, often without a clear physical cause. While not life-threatening, it can seriously affect quality of life and often requires long-term symptom management.
- Celiac disease: This autoimmune condition triggered by gluten can cause severe bloating, malabsorption, and weight loss. Diagnosis is confirmed with antibody tests and intestinal biopsy. Imagine your immune system mistakenly treating gluten like a dangerous invader, attacking your own small intestine in the process. Left untreated, it can lead to anemia, osteoporosis, infertility, and even certain cancers.
- Small Intestinal Bacterial Overgrowth (SIBO): An abnormal increase in gut bacteria in the small intestine can cause bloating, especially after eating. Breath tests are commonly used to detect SIBO. Picture bacteria setting up camp where they don’t belong—right in the small intestine—leading to fermentation, gas, and discomfort soon after meals. If untreated, SIBO can cause nutrient deficiencies and chronic digestive issues.
- Gastroparesis: Often linked to diabetes, this condition slows down stomach emptying, leading to persistent bloating and early satiety. Think of your stomach as a conveyor belt that’s suddenly slowed to a crawl—food lingers too long, causing pressure and nausea. It can lead to malnutrition, weight loss, and poor blood sugar control if unmanaged.
- Gynecological issues: Endometriosis, ovarian cysts, and fibroids can also result in bloating and pelvic discomfort. These conditions are like uninvited guests in the pelvic area, pressing on digestive organs and nerves. Depending on the cause, they can range from mild to severely painful, and sometimes mimic gastrointestinal symptoms.
Each of these conditions has its own diagnostic criteria and treatment strategies, so it’s essential to work with a healthcare provider for proper evaluation.
Diagnosis: Pinpointing the Culprit
Finding the cause of bloating and abdominal pain requires a step-by-step approach, starting with a detailed medical history and dietary review. Here’s a breakdown of the most commonly used diagnostic tools:
| Diagnostic Test | How It Works | Accuracy (1–10) | Average Cost (USD) |
|---|---|---|---|
| Lactose hydrogen breath test | Measures hydrogen in breath after lactose ingestion | 7–8 | $150–$250 |
| SIBO breath test | Measures hydrogen/methane after glucose/lactulose | 6–8 | $200–$350 |
| Abdominal ultrasound | Imaging for structural abnormalities | 6–7 | $300–$600 |
| Endoscopy/Colonoscopy | Visualizes GI tract with biopsies if needed | 9 | $1,000–$3,000 |
| Celiac antibody panel + biopsy | Blood tests plus duodenal biopsy | 9–10 | $400–$2,000 |
Reyus Mammadli, medical consultant, recommends starting with the least invasive methods such as breath tests before progressing to scopes and imaging, especially in younger patients without alarming symptoms.
What to Expect From Each Diagnostic Method:
- Lactose hydrogen breath test: You’ll drink a lactose-containing beverage, then breathe into a tube at intervals. The test measures hydrogen in your breath, which increases if lactose isn’t properly digested. It’s noninvasive and takes about 2–3 hours.
- SIBO breath test: Similar to the lactose test, but uses glucose or lactulose instead. You’re asked to follow a special diet the day before. The test checks for gases like hydrogen and methane to identify bacterial overgrowth in the small intestine.
- Abdominal ultrasound: A technician glides a handheld probe over your belly with some gel to create internal images using sound waves. It’s painless, takes around 30 minutes, and is helpful for detecting cysts, fluid, or organ issues.
- Endoscopy/Colonoscopy: These involve a thin, flexible tube with a camera inserted through the mouth (endoscopy) or rectum (colonoscopy) while you’re sedated. They allow doctors to view the digestive tract and take biopsies if needed.
- Celiac antibody panel + biopsy: First, a blood test checks for antibodies linked to celiac disease. If positive, a follow-up endoscopy may be done to collect tissue samples from your small intestine to confirm the diagnosis.
Real-Life Case Studies: From Mystery to Clarity
Case #1: A 42-year-old woman from Tucson, Arizona, had been battling daily bloating for nearly two years. Despite trying every over-the-counter remedy, nothing helped. After seeing a gastroenterologist and undergoing a SIBO breath test, she was diagnosed with SIBO and treated with rifaximin. Within weeks, her symptoms drastically improved.
Case #2: A 28-year-old male from Brooklyn, New York, experienced severe post-meal bloating and fatigue. Lab work revealed iron-deficiency anemia, and further testing confirmed celiac disease. After eliminating gluten, his energy levels returned and the bloating resolved.
Case #3: A 55-year-old woman in Jacksonville, Florida, complained of lower abdominal pain and bloating for months. Imaging revealed a large ovarian cyst. After surgical removal, her symptoms disappeared.
These examples show the importance of not brushing off chronic bloating—it could be your body waving a red flag.
Cutting-Edge Treatments That Actually Work
Modern medicine is making strides in managing bloating and associated pain. Here are a few standout innovations:
- Rifaximin: A non-absorbable antibiotic used for SIBO and IBS with diarrhea. Clinical trials show up to 40% symptom relief after 2 weeks of treatment ⧉. It works by reducing bacterial overgrowth in the small intestine, often providing fast relief. The average cost for a full course is approximately $1,200 without insurance.
- Low-FODMAP diet apps: Tools like the Monash University FODMAP app help users identify and avoid trigger foods. These apps guide patients through an elimination diet and reintroduction process, improving symptoms in 70–80% of IBS sufferers. Most apps are available for under $10 as a one-time purchase.
- Probiotics: Certain strains, such as Bifidobacterium infantis 35624, have been shown to significantly reduce bloating in IBS patients ⧉. These beneficial bacteria help restore gut flora balance, often easing symptoms within 4–6 weeks. A one-month supply typically costs between $30 and $60.
- Biofeedback therapy: Helps patients with pelvic floor dysfunction to retrain muscles for better bowel movements. Sessions use sensors and visual feedback to improve coordination of abdominal and pelvic muscles. A full course may cost $1,500–$3,000 depending on location and provider.
- SmartPill: A capsule that records pressure, pH, and temperature as it moves through the GI tract, helping diagnose motility disorders ⧉. It’s a noninvasive alternative to traditional motility studies and offers results in real-time. Costs generally range from $1,500 to $3,500.
Newer interventions are being researched, including gut-directed hypnotherapy and microbiome modulation therapies, though more evidence is needed.
Editorial Advice
Don’t let bloating steal your joy—or your jeans’ waistband. Mild occasional bloating is common, but persistent discomfort deserves a deeper look. Tracking your symptoms, noting food patterns, and consulting your physician are key first steps.
Reyus Mammadli, medical consultant, emphasizes: “Patients often think bloating is just about diet, but it can be much more complex. Never ignore persistent symptoms, especially if they’re new or worsening.”
To help your gut, consider a food diary, limit high-FODMAP foods, and avoid gulping air through straws or chewing gum. Stay active—gentle walking after meals can help reduce bloating by stimulating digestion.
Source: iythealth.com
Remember, your gut has a way of telling you what it likes—and what it doesn’t. Listen carefully, and it just might thank you with a little peace and quiet.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.