Eczematous dermatitis, commonly known as eczema, is a condition characterized by red, inflamed, and itchy skin. But why is it so common? In the United States alone, over 31 million people live with some form of eczema, and the prevalence is increasing due to rising pollution levels, climate changes, and genetic factors. The condition is especially common among children, affecting up to 20% of infants, although many eventually outgrow it. For adults, the prevalence hovers around 10%, often related to environmental triggers or other health issues.
Seasonal Flare-Ups of Eczema
| Season | Percentage of Flare-Ups |
|---|---|
| Winter | 45% |
| Spring | 25% |
| Summer | 15% |
| Autumn | 15% |
This chart illustrates the percentage of eczema flare-ups that occur during different seasons. Winter appears to be the most challenging season for those with eczema, likely due to dry air and low humidity levels.
What Causes Eczematous Dermatitis?
The root causes of eczematous dermatitis are complex and often involve an interplay of genetic and environmental factors. Let’s break them down:
- Genetic Predisposition: Research shows that if one parent has eczema, their child has a 50% chance of developing it as well. This genetic link suggests a disruption in the skin barrier, causing it to lose moisture more easily and become more susceptible to irritants.
- Environmental Triggers: Common environmental triggers include pet dander, pollen, mold, and even household cleaning products. Climate also plays a role; low humidity or dry winter air can exacerbate symptoms.
- Immune System Dysfunction: Many individuals with eczema have an overactive immune system that responds to even minor irritations with inflammation. This overreaction causes the skin to break out in rashes and itching, typical symptoms of eczematous dermatitis.
Did You Know? – Eczema in Modern Times
Did you know that a recent study from the National Eczema Association (2023) found that 80% of patients reported a noticeable worsening of their eczema symptoms when experiencing significant stress? Eczema is not just skin deep—it can be closely linked to emotional well-being and overall health.
Psychological Impact of Eczema
| Psychological Effect | Percentage of Patients Affected |
|---|---|
| Anxiety | 50% |
| Depression | 35% |
| Social Isolation | 30% |
| Sleep Disturbances | 55% |
This chart illustrates the psychological impacts commonly associated with eczema. Anxiety and sleep disturbances are prevalent, highlighting the importance of addressing both the physical and emotional aspects of eczema management.
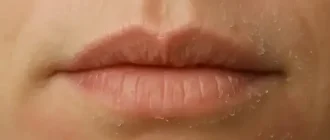
Common Symptoms and How to Recognize Eczema Early
Eczema presents differently in individuals, but common symptoms include:
- Red, inflamed patches on areas like the hands, elbows, knees, and face.
- Intense itching, which can worsen at night and disrupt sleep.
- Dry, cracked skin, sometimes with oozing or bleeding in severe cases.
Identifying these symptoms early can help you manage the condition more effectively. Eczema often has phases of flares and remission, where symptoms come and go over time. It’s critical to take preventive steps during remission to avoid exacerbations.
Factors Contributing to Eczema Flare-Ups
| Trigger Factor | Percentage of Patients Affected |
|---|---|
| Stress | 60% |
| Dry Air / Low Humidity | 50% |
| Allergens (Pollen, Dust Mites) | 40% |
| Harsh Soaps / Detergents | 35% |
| Infections | 20% |
This chart illustrates the most common factors that contribute to eczema flare-ups. Stress and dry air are leading triggers, while allergens and harsh soaps also play a significant role.
How is Eczematous Dermatitis Diagnosed and Treated?
The diagnosis of eczematous dermatitis is usually made through physical examination and medical history. Dermatologists often rule out other skin conditions before confirming an eczema diagnosis.
Treatment Options
- Topical Steroids: These are the most common treatments for reducing inflammation. Mild steroids like hydrocortisone are available over the counter, while stronger versions require a prescription.
- Moisturizers: Keeping the skin hydrated is key. Emollient-rich creams, often containing ceramides, help restore the skin’s natural barrier. Did you know that the average American with eczema spends over $300 annually on skincare products to manage their condition?
- Immunosuppressants: Medications like cyclosporine or methotrexate are sometimes prescribed for severe cases, especially when topical treatments fail.
- Biologic Drugs: The development of biologic drugs like Dupilumab (Dupixent) offers a new treatment avenue for moderate to severe cases. Dupilumab, for example, works by targeting specific proteins in the immune system that trigger eczema symptoms, providing relief for up to 60% of patients within the first 16 weeks.
What Are Natural and Preventive Measures for Managing Eczema?
While conventional treatments are effective, many people also turn to preventive measures to manage symptoms better:
- Avoiding Triggers: Identifying and avoiding personal triggers, such as harsh soaps, fabrics like wool, and allergens like dust mites, is essential for managing flare-ups.
- Humidifiers: Adding moisture to the air can make a significant difference during colder months when heating systems dry out the indoor environment.
- Dietary Adjustments: While there’s no specific diet that cures eczema, some individuals notice an improvement when they cut out common inflammatory foods such as dairy or gluten. Omega-3-rich foods, like fish and flaxseed, may also provide benefits.
A Deep Dive into the Psychological Impact of Eczema
Eczema isn’t just a physical condition—it can have profound psychological impacts, particularly on children and teens. Studies indicate that children with eczema are 20% more likely to develop anxiety or depression due to the social stigma and discomfort associated with visible skin conditions. Adults are not exempt either; many report avoiding social situations due to flare-ups.
What Do Experts Recommend for Long-Term Management?
Long-term management involves a combination of treatment and lifestyle adjustments. Dermatologists often recommend creating a “flare plan,” which includes:
- Daily Skincare Routine: Moisturize within three minutes of bathing to lock in moisture.
- Stress Management: Addressing stress, which is a major trigger, through cognitive behavioral therapy (CBT) or mindfulness techniques.
- Follow-Up Appointments: Regular check-ups with a dermatologist can help adjust treatments as needed. Newer biologics and therapies are continuously evolving, making it crucial to stay updated.
Body Distribution of Eczema
| Body Area | Percentage of Patients Affected |
|---|---|
| Hands | 40% |
| Face and Neck | 30% |
| Elbows and Knees | 25% |
| Feet | 20% |
| Scalp | 15% |
This chart illustrates the common areas of the body affected by eczema. Hands, face, and neck are among the most frequently impacted areas, often leading to significant discomfort and visibility of symptoms.
Is Eczema Curable?
Currently, there is no cure for eczema. However, the good news is that advancements in research are promising, and symptoms can be significantly managed with the right treatment and preventive measures. According to recent statistics, about 50% of children “outgrow” eczema by their teenage years, but for others, it remains a lifelong condition.
The Editorial Team’s Advice
If you or a loved one suffers from eczematous dermatitis, start by consulting a dermatologist for a tailored treatment plan. Stick to simple, fragrance-free skincare products and keep track of your triggers. Don’t forget to moisturize often and avoid scratching. A consistent approach can make a world of difference in reducing flare-ups and improving quality of life.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.