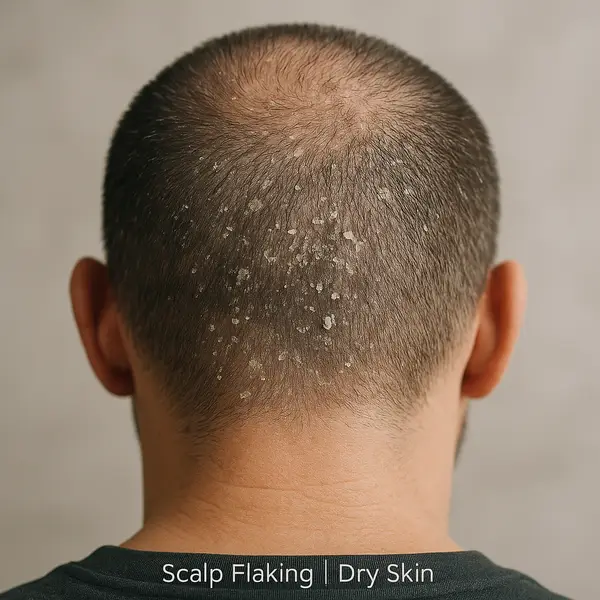
At first glance, dead skin on the scalp might seem like just a harmless case of dandruff — a little flaking, maybe some itching, nothing too dramatic. But here’s the twist: when it goes beyond those light, snowy flakes and turns into thick patches or persistent scaling, your scalp could be sounding the alarm on something more serious.
You might notice it as fine white specks on your black shirt, waxy buildup along your hairline, or even hard plaques that resist every wash. Each type of flaking tells a different story — and knowing which one you’re dealing with is the first step toward treating it right.
According to a 2023 survey conducted by the American Academy of Dermatology, around 1 in 5 Americans reports regular scalp flaking or scaling. That’s nearly 66 million people dealing with some form of dead skin buildup ⧉.
What Causes Dead Skin on the Scalp?
Dead skin on the scalp is not just about bad hygiene. In fact, it’s often more about biology than behavior. Here are the most common culprits, along with what they feel like and how seriously they can affect your scalp health:
Seborrheic Dermatitis
Think of this like your scalp reacting to everyday yeast like a drama queen — something normal suddenly gets wildly out of control. Seborrheic dermatitis is caused by an overgrowth of Malassezia, a yeast that normally lives peacefully on the skin. When triggered by stress, cold weather, or hormonal shifts, it leads to greasy, inflamed patches and yellowish flakes.
Impact scale: 6/10 – Uncomfortable, recurring, but manageable with the right shampoo. It’s like driving through a neighborhood with lots of potholes: annoying, but you’ll get there.
Psoriasis
This is your immune system mistaking your scalp for an intruder and attacking it. Scalp psoriasis results in thick, silvery scales that may go beyond the hairline. It’s not just flaky — it’s itchy, tight, and sometimes painful.
Impact scale: 8/10 – Chronic and stubborn. Like a broken thermostat that keeps turning on the heat — it’s manageable but needs consistent attention.
Contact Dermatitis
Sometimes the problem is something you’ve added to your routine: a new shampoo, hair dye, or styling gel. The scalp responds with inflammation, redness, and itching, like a mini protest against an irritating ingredient.
Impact scale: 4/10 – Short-term and reversible. It’s like wearing an itchy sweater — take it off, and you’re good.
Fungal Infections
Tinea capitis, commonly called ringworm of the scalp, is a contagious fungal infection that often causes patchy hair loss, redness, and scaling. It’s more common in kids but adults aren’t immune.
Impact scale: 7/10 – Highly treatable, but uncomfortable and contagious. Imagine a skin version of a cold — annoying and easily shared.
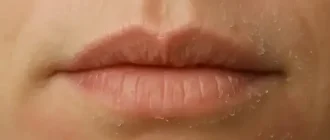
Dry Skin
Sometimes the culprit is just simple dryness. Whether it’s due to cold weather, over-washing, or low humidity, dry skin leads to fine, white flakes that are less greasy and more like dandruff.
Impact scale: 3/10 – Mild and manageable. Like having chapped lips — easy to fix, but uncomfortable if ignored.
Case Study
A 42-year-old male from Flagstaff, AZ, presented with persistent flaking and itching around the crown of his head. Despite switching shampoos multiple times, symptoms worsened. A dermatologist diagnosed seborrheic dermatitis and prescribed ketoconazole 2% shampoo. Symptoms improved within 10 days of consistent use.
Diagnosing the Problem: From Microscopes to Modern Tech
Getting to the root (pun intended) of dead scalp skin isn’t always straightforward. Here’s how professionals figure it out:
| Diagnostic Method | Accuracy (1-10) | Average Cost (USD) |
|---|---|---|
| Visual Exam | 6 | $100–$150 |
| Skin Scraping & Culture | 8 | $70–$120 |
| Scalp Biopsy | 9 | $300–$500 |
| Reflectance Confocal Microscopy (RCM) | 8 | $250–$400 |
Advanced tools like RCM are becoming more accessible in urban clinics and provide near-cellular imaging without needing to cut into the skin ⧉.
What Each Diagnostic Method Involves
Visual Exam – A dermatologist uses a dermatoscope to inspect your scalp. This tool magnifies the surface and helps reveal signs of inflammation, scaling, or unusual pigmentation. It’s painless, fast (under 10 minutes), and often done during your first visit. Results are immediate, but the accuracy depends largely on the clinician’s experience.
Skin Scraping & Culture – A small sample of skin is gently scraped from the scalp using a sterile blade or slide. It’s not painful, though you may feel slight pressure. The sample is then sent to a lab to grow any potential fungal or bacterial organisms. Results usually take 3–7 days. This method is quite accurate for diagnosing fungal infections.
Scalp Biopsy – This involves removing a tiny piece of scalp tissue (usually 4mm) under local anesthesia. It may sting briefly during the numbing process, but you won’t feel the actual removal. The sample is sent to a lab for histopathological analysis. Results typically take 1–2 weeks. This method is especially valuable when autoimmune or cancerous causes are suspected.
Reflectance Confocal Microscopy (RCM) – RCM is a non-invasive, high-resolution imaging technique. A flat scanner is gently placed on the scalp, which captures microscopic images in real time — almost like a live MRI for your skin. Totally painless, with results available immediately during the exam. Ideal for monitoring chronic scalp disorders without needing a biopsy.
What Actually Works? Treatment Options That Deliver
Let’s talk solutions — and not just the ones that make your bathroom shelf prettier. Here are evidence-backed treatments, with what you actually need to know about how to use them, what to expect, and whether they’ll work for you:
Medicated Shampoos
These are often the first line of defense. Look for active ingredients like ketoconazole (antifungal), zinc pyrithione (antibacterial and antifungal), coal tar (slows down skin cell growth), or salicylic acid (breaks down scales).
Most products like Nizoral, Neutrogena T/Gel, and Head & Shoulders Clinical Strength should be used 2–3 times per week. To get results, let the shampoo sit on your scalp for 3–5 minutes before rinsing — treat it like a mask, not a rinse-and-go.
Treatment may take 2–4 weeks to show visible improvement. Costs range from $8 to $25. This method is very effective for seborrheic dermatitis and mild psoriasis but may not resolve deeper autoimmune or fungal conditions.
Topical Corticosteroids
For severe inflammation and stubborn plaques, corticosteroids like clobetasol propionate (available in foam, gel, or liquid) can drastically reduce redness, swelling, and itching within days.
Typically, doctors recommend using them once daily for 1–2 weeks. It’s a short-term rescue — perfect for flare-ups but not a maintenance solution.
While extremely effective for autoimmune conditions like scalp psoriasis or lupus, long-term use can thin the skin. Cost with prescription averages between $30–$70. Cost (with prescription): around $30–$70.
Antifungal Creams
When a fungal infection like tinea capitis is the culprit, topical antifungal agents such as terbinafine or ciclopirox are usually prescribed.
These creams are applied once or twice a day, typically for 7–14 days. Most people begin noticing relief within the first week.
They’re very effective — but only if the issue is fungal. If the underlying cause is autoimmune or inflammatory, they won’t help. Tubes usually cost $15–$40.
Laser Therapy
Low-level laser therapy (LLLT) uses red light to reduce inflammation and speed up healing of the scalp. It’s painless, non-invasive, and often used alongside other treatments.
Devices like iRestore or Capillus use helmet or comb designs and are FDA-cleared. Sessions last 15–30 minutes, done 3–4 times per week. Results generally appear after 2–3 months.
It’s ideal for people dealing with chronic conditions like psoriasis or dandruff who also want to improve hair growth. However, with prices ranging from $400 to $1,500, it’s a longer-term investment.
Natural Oils (With Caution)
Natural oils like tea tree, coconut, and jojoba have moisturizing or antifungal properties that can benefit a dry or flaky scalp.
Tea tree oil has been shown to reduce the yeast that contributes to dandruff, but it must be diluted. Mix 2–3 drops with a tablespoon of a carrier oil (like jojoba or olive) and massage into the scalp once or twice weekly.
While suitable for mild cases or as maintenance therapy, these oils are not a cure. Always patch test first ⧉ — especially for sensitive skin types.
Is It Something More Serious?
Sometimes, dead skin isn’t just about skin. Scalp issues can be a sign of:
- Lupus (especially discoid lupus) – This is an autoimmune disease where the immune system attacks the skin, leading to red, scaly plaques that can scar and cause permanent hair loss. These patches are often resistant to over-the-counter treatments and tend to worsen with sun exposure.
- Lichen planopilaris – A rare inflammatory condition that damages hair follicles, leading to patchy bald spots and permanent hair loss if left untreated. Symptoms often include intense itching or burning, and the skin can appear shiny or scarred.
- Skin cancer (very rare, but possible) – In rare cases, persistent, crusty, or bleeding patches on the scalp that don’t heal could indicate basal or squamous cell carcinoma. Early detection is critical, as these cancers are treatable if caught before they spread.
If you notice bleeding, rapid thickening of plaques, or hair loss that spreads fast — don’t wait. Get a professional opinion.
In one case, a 34-year-old woman from Atlanta, GA developed persistent, thick plaques behind her ears and along the nape. A biopsy confirmed discoid lupus. Early intervention prevented permanent scarring and hair loss.
How to Keep the Scalp in Good Shape
Prevention may not sound sexy, but it works. Here are a few smart habits — with details on how and why to actually make them work for you:
- Wash your scalp regularly — not just your hair. Many people forget that cleansing the scalp is just as important as shampooing strands. Use your fingertips (not nails) to massage the scalp gently with a dermatologist-recommended shampoo, ideally 2–3 times a week. For oily scalps or those prone to seborrheic dermatitis, this could mean daily gentle washing. If you have dry or curly hair, aim for twice a week to avoid overdrying.
- Use lukewarm water (not hot!) to avoid stripping natural oils. Hot water might feel relaxing, but it strips the scalp of sebum — its natural protective oil. Lukewarm (about 98°F / 37°C) water helps cleanse without causing dryness or irritation. This tip is especially important for people with eczema-prone or psoriasis-affected scalps.
- Avoid overusing styling products that clog pores. Gels, waxes, dry shampoos, and hairsprays can build up over time and create a film that prevents the scalp from breathing. If you style your hair daily, opt for non-comedogenic, water-soluble products and use a clarifying shampoo once weekly to detox the scalp. Great for oily and acne-prone skin types.
- Eat a diet rich in omega-3s, zinc, and B vitamins ⧉. Your scalp’s condition reflects what’s going on inside your body. Omega-3s (found in fish, flaxseed, walnuts), zinc (pumpkin seeds, lentils), and B vitamins (leafy greens, eggs) support skin regeneration, reduce inflammation, and strengthen the scalp barrier. Ideal for those with recurring flaking or scalp sensitivity.
- Don’t scratch — it only makes things worse. While it’s tempting, scratching inflames the scalp, damages the protective barrier, and can even lead to infections or scarring. Instead, soothe the itch with cool compresses, over-the-counter hydrocortisone, or medicated shampoos. This advice is particularly crucial for anyone managing dermatitis or psoriasis.
And here’s the kicker: get your scalp checked at least once a year if you’ve had chronic issues before.
And here’s the kicker: get your scalp checked at least once a year if you’ve had chronic issues before.
Editorial Advice
Dead skin on the scalp isn’t just about snowflakes on your shoulders — it’s about skin health and overall wellbeing. Reyus Mammadli, medical consultant, recommends early diagnosis and tailored treatment over one-size-fits-all remedies: “Your scalp deserves the same attention as your skin — it’s skin, after all.”
Don’t let embarrassment keep you from seeing a dermatologist. New diagnostic tools and treatments are making scalp care more precise and effective than ever before. Whether it’s a quick shampoo fix or something more complex, there’s a solution waiting — and it’s probably easier than you think.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.