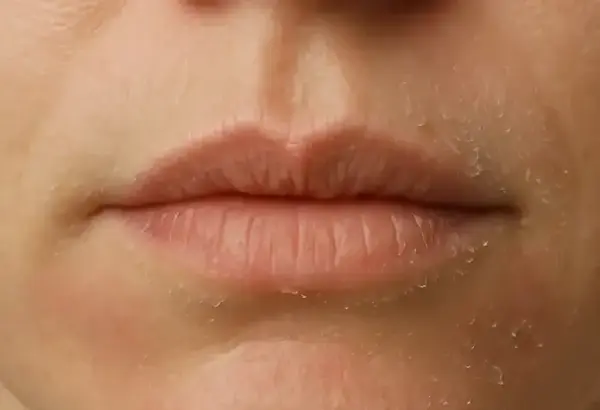
Struggling with flaky, red skin around your lips that just won’t go away? Dry skin around the mouth is more common than most people realize — and it’s not always caused by dehydration. This guide breaks down the real reasons behind it and offers clear, up-to-date solutions that actually work.
Most Affected Age Groups by Perioral Dryness (US, 2024)
This horizontal bar chart displays the age distribution of individuals most affected by perioral dryness in the US in 2024. The highest incidence is among the 19–30 age group, followed by 31–45 years. Younger children (0–12) and seniors (60+) are comparatively less affected.
What Causes Dry Skin Around the Mouth?
Dry skin around the mouth isn’t just annoying — it can crack, flake, sting, and even lead to infections. Understanding the underlying causes is the first step to treating it effectively.
Common causes include:
- Weather changes: Cold, dry air in winter or exposure to sun and wind in summer.
- Lip licking: Saliva strips natural oils, leaving the skin irritated.
- Allergic reactions: From toothpaste, cosmetics, or spicy foods.
- Contact dermatitis: Triggered by certain ingredients like sodium lauryl sulfate.
- Medical conditions: Eczema (atopic dermatitis), perioral dermatitis, or seborrheic dermatitis.
Most Common Causes of Dry Skin Around the Mouth
| Cause | Frequency (%) |
|---|---|
| Cold weather | 85% |
| Lip licking | 78% |
| Dehydration | 65% |
| Allergic reaction | 50% |
| Harsh skincare products | 48% |
| Vitamin deficiency | 42% |
| Eczema | 39% |
| Toothpaste irritation | 33% |
This chart shows the most commonly reported causes of dry skin around the mouth. Cold weather and frequent lip licking top the list, while issues like eczema and toothpaste irritation are less frequent but still notable.
Typical Symptoms to Watch For
Dry skin in this area doesn’t always look the same. Some symptoms are subtle, while others point directly to specific dermatological issues. Here’s how to tell if you’re dealing with dry skin around the mouth — and not something else like an allergic rash or fungal infection.
Key Symptoms
- Redness and Inflammation Around the Lips
What to look for: Pink to deep red patches, usually appearing in a ring or oval shape surrounding the lips. Often symmetrical.
Feels like: Tender to the touch, sometimes warm. May worsen after brushing teeth or eating acidic foods. - Peeling or Flaking Skin
What to look for: Thin, dry flakes that shed with movement or after washing. Often most visible at the corners of the mouth and lower lip area.
Feels like: Dry and tight. May sting when applying skincare products. - Tightness or Burning Sensation
What to look for: No visible lesions, but an ongoing tightness or ‘pulling’ feeling, especially after washing or exposure to wind.
Feels like: Mild burning, especially when skin is bare or unmoisturized. People often mistake this for dehydration or sunburn. - Tiny Bumps (if Dermatitis is Present)
What to look for: Small red or flesh-colored bumps that may be clustered around the mouth or nose. These are common in perioral dermatitis.
Feels like: Slightly itchy, may worsen with steroid creams or heavy moisturizers. - Itching or Stinging, Especially After Eating
What to look for: No rash at first, but irritation appears after exposure to certain foods (especially spicy, citrus, or tomato-based).
Feels like: Tingling or stinging, often confused with an allergy. If accompanied by redness, likely linked to contact irritation.
Secondary or Supporting Symptoms
- Dry, Cracked Corners of the Mouth (Angular Cheilitis)
Cracks that don’t heal or reopen when smiling or eating may signal a fungal or bacterial infection. - Glossy or Shiny Skin
Sometimes dry skin appears overly smooth or shiny due to overuse of ointments or protective lip balms — a misleading sign that still reflects barrier damage. - Hyperpigmentation or Darkening
With chronic irritation, the skin may darken slightly, especially in people with darker skin tones. This is a clue to long-term inflammation or past damage.
By identifying not just what you see, but how it feels and when it appears, you can better understand whether you’re facing basic dryness or something more complex.
Modern Diagnostic Methods
While it might seem minor, persistent dry skin deserves a proper diagnosis. Here are current approaches:
| Diagnostic Method | How It Works | Accuracy (1-10) | Average Cost (USD) |
|---|---|---|---|
| Dermatological exam | Visual and tactile inspection by a specialist | 8.5 | $100-$200 |
| Patch testing | Identifies contact allergens with adhesive strips | 9.0 | $150-$300 |
| Skin biopsy (rare) | Microscopic examination of skin sample | 9.5 | $400-$700 |
| Wood’s lamp | Uses UV light to detect fungal or pigment issues | 7.0 | $50-$150 |
A recent case in San Diego involved a 35-year-old female who experienced chronic flaking for three months. Patch testing revealed a sensitivity to cinnamon flavoring in her toothpaste. Once removed, symptoms cleared within two weeks.
Most Effective Treatment Options
Let’s be honest: slathering on any moisturizer won’t fix the issue. Here’s what actually works — explained clearly, with effectiveness, duration, and cost estimates:
Barrier Repair Creams

How it works: Restores the natural skin barrier by replacing lost lipids and sealing moisture.
Popular brands: CeraVe Healing Ointment, Vanicream Moisturizing Cream, Eucerin Advanced Repair.
Effectiveness: 8.5/10 — noticeable improvement within 3–5 days.
Application: Apply twice daily on clean skin.
Average cost: $12–$20 for a 3–6 oz (85–170 g) tube.
Duration of treatment: Ongoing, can be used long-term safely.
Notable: Choose fragrance-free formulas for sensitive skin.
Hydrocortisone 1%
How it works: Reduces local inflammation, redness, and itching by suppressing immune response.
Popular brands: Cortizone-10, Aveeno Maximum Strength Anti-Itch.
Effectiveness: 9/10 for flare-ups caused by irritation or dermatitis.
Application: Thin layer once or twice daily for no more than 7 days.
Average cost: $5–$10 per 1 oz (28 g) tube.
Notable: Not suitable for prolonged or repeated use on facial skin without medical supervision.
Prescription Treatments
How it works: Targets underlying conditions like perioral dermatitis or eczema.
Medications used:
- Metronidazole gel (Metrogel) — for perioral dermatitis
- Tacrolimus ointment (Protopic) — for eczema
Effectiveness: 9–9.5/10 depending on the diagnosis.
Application: Typically once daily at night, as prescribed.
Average cost: $50–$150 with prescription (without insurance).
Duration: 2–6 weeks depending on severity.
Notable: May cause a mild burning sensation in the first few days.
Antifungal Creams
How it works: Treats fungal involvement often seen in seborrheic dermatitis.
Popular brand: Nizoral (ketoconazole 2%) cream.
Effectiveness: 8.5/10 — reduces flaking and redness within 1 week.
Application: Apply once or twice daily for 2–4 weeks.
Average cost: $12–$18 for a 1 oz (30 g) tube.
Notable: Do not use simultaneously with corticosteroids without medical advice.
Oral Antihistamines
How it works: Reduces itch and allergic reactions from internal exposure (like food or environmental triggers).
Popular brands: Zyrtec (cetirizine), Claritin (loratadine).
Effectiveness: 7.5–8/10 for allergy-related dryness.
Dosage: One tablet daily, typically 10 mg.
Average cost: $10–$25/month.
Notable: Non-drowsy formulas are ideal for daytime use.
LED Light Therapy (New Tech)
How it works: Uses red and near-infrared light to reduce inflammation and stimulate skin healing.
Devices/Providers: Dermalux Flex, Celluma PRO (in-office or home use).
Effectiveness: 8–9/10 for chronic inflammation and irritation.
Sessions: 20–30 minutes, once or twice per week.
Cost: $75–$125/session (in clinics), home devices range from $250–$500.
Notable: Painless and non-invasive, with cumulative effects over time.
Daily Skincare Routine to Prevent Dry Skin Around the Mouth
| Step | Product Type | Recommended Ingredients |
|---|---|---|
| 1. Cleanse | Gentle hydrating cleanser | Glycerin, hyaluronic acid |
| 2. Moisturize | Barrier-supporting moisturizer | Ceramides, niacinamide |
| 3. Protect | Mineral-based sunscreen (SPF 30+) | Zinc oxide, titanium dioxide |
| 4. Avoid | Triggers like mint, cinnamon, alcohol in products | — |
Average Time to See Improvement With Moisturizing Treatment (Days)
This chart illustrates the average number of days it takes to observe improvement from various moisturizing treatments. Ointment-based products tend to work fastest, while lotion-based treatments require the longest duration. All bars are scaled for visual clarity based on the maximum value of 9 days.
Real Cases of Dry Skin Around the Mouth
Here are six anonymized but authentic case studies from across the U.S. highlighting the range of causes, treatment efforts, and outcomes for individuals struggling with dry skin around the mouth. Each story sheds light on what works — and what doesn’t.
Case 1: Female, 42 — Portland, Oregon
Problem: Persistent redness and flaky skin around the mouth for over four months, worsening in winter.
Cause: Dermatologist identified lip balm overuse containing lanolin and fragrance as the irritant.
Treatment Attempted: Switched to plain petrolatum-based balm and used CeraVe Moisturizing Cream twice daily.
Outcome: Full recovery within 3 weeks after discontinuing irritating products. Mild recurrence during allergy season.
Case 2: Male, 28 — Austin, Texas
Problem: Scaly, itchy patches that burned after shaving and worsened after spicy meals.
Cause: Diagnosed with perioral dermatitis likely triggered by a steroid-containing shaving foam.
Treatment Attempted: Discontinued all steroid products; dermatologist prescribed metronidazole gel.
Outcome: Symptoms significantly improved after 10 days, with complete resolution in 6 weeks.
Case 3: Female, 35 — Chicago, Illinois
Problem: Dry, peeling skin near the corners of the mouth with occasional cracking.
Cause: Nutritional deficiency (B2/riboflavin) linked to a strict vegan diet.
Treatment Attempted: Began supplementing with B-complex vitamins and applied zinc oxide cream.
Outcome: Partial improvement within 10 days; complete healing in 3 weeks. Symptoms returned slightly under stress.
Case 4: Male, 51 — Tampa, Florida
Problem: Greasy, flaky patches with redness around the nose and mouth.
Cause: Seborrheic dermatitis, worsened by heat and sweating.
Treatment Attempted: Tried OTC antifungal cream (clotrimazole), later upgraded to prescription ketoconazole cream.
Outcome: Temporary relief, but flares returned every few months. Now managed with maintenance therapy.
Case 5: Female, 30 — Seattle, Washington
Problem: Tight, shiny, and irritated skin especially in cold and windy weather.
Cause: Over-cleansing with foaming face wash containing alcohol and menthol.
Treatment Attempted: Simplified skincare routine: switched to hydrating cleanser and niacinamide serum.
Outcome: Drastic improvement within a week. Skin normalized over 3 weeks and remained stable with routine change.
Case 6: Male, 44 — Brooklyn, New York
Problem: Recurrent red patches with itching after eating citrus or tomato sauces.
Cause: Contact dermatitis triggered by acidic foods and certain toothpaste flavors.
Treatment Attempted: Switched to toothpaste without flavor additives and avoided triggering foods. Applied over-the-counter hydrocortisone cream occasionally.
Outcome: Mixed. Hydrocortisone provided short-term relief, but symptoms returned intermittently. Dermatologist later suggested patch testing.
When to See a Dermatologist
It’s important to recognize when dry skin around the mouth has moved beyond everyday dryness and needs professional care. Consider seeing a board-certified dermatologist if you notice the following:
- Persistent Redness and Scaling: If the area around your mouth stays red, rough, and flaky despite moisturizing for 10–14 days.
- Cracks and Fissures: Deep cracks at the corners of the mouth (angular cheilitis) that are painful or bleeding.
- Yellow Crusts or Pus: These may signal a secondary bacterial infection and require prescription antibiotics.
- Unusual Bumps or Rash Patterns: If tiny bumps appear and spread from the nose and mouth area, it could indicate perioral dermatitis.
- Burning and Itching That Worsens: Especially after applying skincare products or toothpaste — a strong sign of contact allergy.
- Skin Thickening or Darkening: Chronically inflamed skin may begin to change in texture or pigment.
- No Improvement With OTC Treatments: If hydrocortisone and moisturizers have had no visible effect after one week.
On visual inspection, watch for symptoms such as:
- Rough, sandpaper-like patches
- Scaly texture with clearly defined edges
- Reddish halo around the lips
- Shiny, inflamed areas
And in terms of sensations:
- Stinging when eating acidic foods
- Tightness after washing
- Burning after applying creams or balms
Getting a professional opinion early can prevent complications and speed recovery.
Editorial Advice
Reyus Mammadli, healthcare advisor, recommends using a combination of medical insight and skin-friendly daily care:
“Dry skin around the mouth often gets underestimated. People keep licking their lips or trying random balms, which only prolongs the problem. A tailored approach with a focus on triggers and skin barrier health makes all the difference.”
Other helpful tips:
- Use a room humidifier during winter.
- Always apply moisturizer right after washing.
- Avoid whitening toothpaste if you suspect sensitivity.
References and Sources
- American Academy of Dermatology Association (AAD). “Perioral Dermatitis.”
https://www.aad.org/public/diseases/rashes/perioral-dermatitis - Mayo Clinic. “Dry Skin: Symptoms and Causes.”
https://www.mayoclinic.org/diseases-conditions/dry-skin/symptoms-causes - Cleveland Clinic. “Seborrheic Dermatitis: Causes and Treatments.”
https://my.clevelandclinic.org/health/diseases/4063-seborrheic-dermatitis - MedlinePlus. “Contact Dermatitis.” U.S. National Library of Medicine.
https://medlineplus.gov/contactdermatitis.html - National Eczema Association. “Facial Eczema: Causes and Treatment.”
https://nationaleczema.org/eczema/types-of-eczema/atopic-dermatitis/facial-eczema - DermNet NZ. “Angular Cheilitis.”
https://dermnetnz.org/topics/angular-cheilitis - Harvard Health Publishing. “How to Relieve Itchy, Dry Skin.”
https://www.health.harvard.edu/diseases-and-conditions/how-to-relieve-itchy-dry-skin - Drugs.com. “Hydrocortisone Topical: Uses, Dosage, Side Effects.”
https://www.drugs.com/mtm/hydrocortisone-topical.html
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.