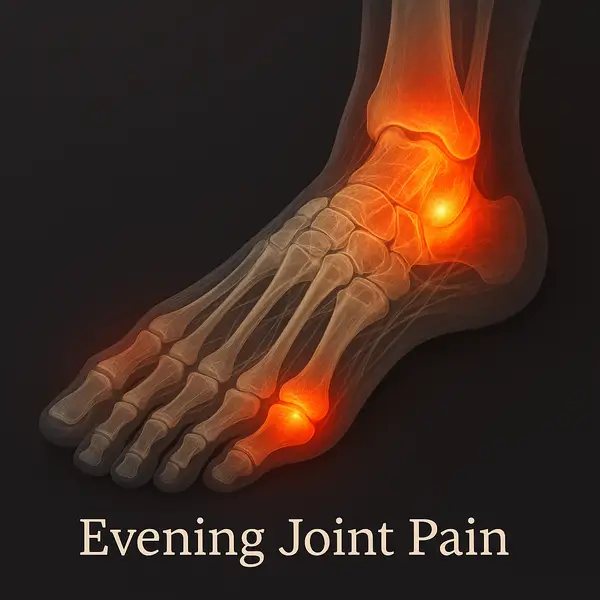
Ever get that nagging ache in your feet right around dinnertime? You’re not alone. Evening foot joint pain refers to discomfort, stiffness, or swelling in the joints of the feet—most often in the toes, arches, or ankles—that tends to worsen as the day winds down. It’s particularly common in people who are on their feet all day or those with underlying conditions like arthritis or gout.
The pain usually presents as a dull throbbing or sharp stinging sensation and may come with swelling or redness. While it can affect anyone, individuals aged 40 and older report it more frequently. For Americans juggling long work hours and active lifestyles, this is more than just an inconvenience—it’s a quality-of-life issue.
Why Do Feet Hurt More in the Evenings?
Let’s get into the science (without putting you to sleep). During the day, our feet absorb shock and pressure from walking, standing, or even just balancing our body weight. That cumulative stress catches up by evening. As circulation slows down later in the day, inflammation tends to pool in the extremities, especially the feet.
Below are the most common underlying reasons why that evening pain hits hard:
Osteoarthritis or Rheumatoid Arthritis
Both conditions cause inflammation and degeneration in joints—but in different ways. Osteoarthritis is wear-and-tear, while rheumatoid arthritis is autoimmune.
Symptoms: Morning stiffness that lasts more than 30 minutes, reduced joint flexibility, swelling, and deep aching pain that worsens with use.
Type of pain: Aching, grinding, and stiffness by evening. You may also feel your feet are “locking up.”
Other signs to look for: Difficulty climbing stairs, fatigue, and sometimes joint redness. Swelling may fluctuate throughout the day.
How serious: High. If left untreated, joint damage becomes irreversible. Don’t delay seeking a rheumatologist’s opinion.
Analogy: Imagine your joints as hinges on an old door—they squeak more at the end of the day from overuse.
Plantar Fasciitis
This condition affects the thick band of tissue that runs along the bottom of your foot (the plantar fascia). It becomes inflamed from overuse or poor arch support.
Symptoms: Sharp heel or arch pain, especially during the first few steps in the morning or after rest. Gets worse again by evening after activity.
Type of pain: Stabbing, especially in the heel or mid-foot.
Other signs: Tenderness when pressing the arch, or pain when standing after sitting.
How serious: Moderate. Can be managed conservatively but may require physical therapy if persistent.
Analogy: Like overstretching a tight rubber band every day—it eventually snaps back in protest.
Gout Flare-Ups
Gout is a form of inflammatory arthritis caused by excess uric acid crystallizing in joints—most often in the big toe.
Symptoms: Sudden, severe pain, often at night, with redness, heat, and swelling.
Type of pain: Intense, burning, and often intolerable.
Other signs: Difficulty wearing shoes, sensitivity to touch, and visible joint inflammation.
How serious: High during a flare-up. Gout can lead to joint destruction if attacks are frequent.
Analogy: It feels like someone lit a match inside your joint—fast and fiery.
Flat Feet or Fallen Arches
Flat feet lack the natural arch that helps absorb shock. Without that, joints and ligaments get overloaded throughout the day.
Symptoms: Foot fatigue, aching arches, shin splints, or knee pain.
Type of pain: Dull aching or cramping by the evening.
Other signs: Feet may turn outward, shoes wear unevenly, or you tire quickly during walking.
How serious: Mild to moderate. Manageable with supportive footwear and inserts.
Analogy: Think of walking on a mattress with no springs—there’s no bounce-back, only pressure.
Improper Footwear
Shoes that lack cushioning or support force your joints to absorb more stress. This includes flip-flops, worn-out sneakers, and high heels.
Symptoms: Generalized foot soreness, toe discomfort, ankle strain.
Type of pain: Sore, tired, and stiff feet at day’s end.
Other signs: Blisters, calluses, altered walking pattern.
How serious: Low to moderate. Easy to fix with better footwear.
Analogy: Imagine running a marathon in slippers—it’s all strain, no support.
A 2023 study published by the American Academy of Orthopaedic Surgeons found that over 62% of adults with sedentary desk jobs still experience end-of-day foot pain, largely due to poor posture and inadequate foot ⧉.
How Is It Diagnosed?
Identifying the root cause is key, and doctors typically use a combination of:
- Physical Examination: Your provider checks for swelling, tenderness, and mobility. This is a quick, non-invasive process involving touch and guided movements. You may be asked to walk or flex your foot. No pain beyond what you already feel is typically caused during this check.
- X-rays: Good for spotting fractures, arthritis, or bone spurs. You’ll lie or sit still while your foot is positioned under the machine—takes only a few minutes and is completely painless. Accuracy: 7/10. Cost: ~$100–250 (approx. €90–230).
- MRI or Ultrasound: These pick up soft tissue damage, including ligament tears or inflammation. Ultrasound involves a probe gliding over your skin with gel (no discomfort), while MRI requires lying still inside a large machine for up to 30 minutes. It’s non-invasive, but some people feel claustrophobic. Accuracy: 9/10. Cost: ~$500–1,200 (approx. €460–1,100).
- Blood Tests: Used to detect markers of inflammation or uric acid (for gout). A quick blood draw from your arm—minimal discomfort and over in under 5 minutes. Accuracy: 8/10. Cost: ~$50–150 (approx. €45–140).
One case involved a 52-year-old woman from Phoenix, Arizona, who developed persistent foot joint pain every evening. An ultrasound revealed a previously undiagnosed ligament strain combined with early-onset rheumatoid arthritis—something traditional X-rays had missed entirely. An ultrasound revealed a previously undiagnosed ligament strain combined with early-onset rheumatoid arthritis—something traditional X-rays had missed entirely.
What Are the Most Effective Treatments?
Treatment depends on the cause, but let’s explore the most common and effective methods in more detail:
NSAIDs (Nonsteroidal Anti-inflammatory Drugs)
Examples: Ibuprofen (Advil, Motrin), Naproxen (Aleve)
How it works: These medications block enzymes responsible for inflammation, reducing pain and swelling in the joints. They don’t cure the root cause but suppress symptoms effectively—like muting the alarm instead of fixing the fire.
How to use: Oral tablets are taken 1–2 times daily after meals. Topical versions (e.g., Voltaren gel) can be applied directly to painful areas 2–4 times per day.
Effectiveness: 7/10 for short-term relief
Estimated cost: $10–25/month (approx. €9–23)
When to avoid: If you have a history of ulcers, kidney issues, or take blood thinners.
Topical Analgesics
Examples: Diclofenac gel, menthol-based creams (e.g., Biofreeze), capsaicin cream
How it works: These provide localized pain relief by blocking nerve signals or delivering a cooling/warming sensation. Think of it like turning down the volume on a blaring speaker.
How to use: Apply a thin layer over the affected joint 3–4 times a day. Wash hands thoroughly afterward.
Effectiveness: 5–6/10 for mild to moderate pain
Estimated cost: $8–20/tube (approx. €7–18)
Best for: Early-stage arthritis, minor sprains, or when oral NSAIDs aren’t an option.
Orthopedic Shoe Inserts (Insoles)
Types: Custom orthotics, over-the-counter arch support insoles (e.g., Superfeet, Dr. Scholl’s)
How it works: Inserts correct biomechanical imbalances, improve arch support, and reduce joint impact while walking. Imagine adding shock absorbers to your shoes—they reduce wear on the suspension (your joints).
How to use: Worn daily inside shoes, especially during work or long standing.
Effectiveness: 7–8/10 when properly fitted
Estimated cost: $25–60 OTC, $200–500 custom (approx. €23–460)
Compression Socks
How it works: Gentle pressure boosts blood flow, reduces swelling, and supports the joints—especially beneficial if circulation slows in the evening.
How to use: Worn during the day or for several hours after work. Choose medical-grade (15–20 mmHg) for therapeutic effect.
Effectiveness: 6/10
Estimated cost: $15–40/pair (approx. €14–38)
Great for: People with jobs that involve prolonged standing or varicose vein issues.
Targeted Physical Therapy
What it involves: Manual therapy, strengthening exercises, balance work, and foot-specific stretches led by a licensed physical therapist.
How it works: Helps realign joints, improve muscle coordination, and reduce compensatory strain. Unlike painkillers, this method aims to fix the engine—not just silence the noise.
How often: 1–2 sessions/week for 6–8 weeks, plus home exercises
Effectiveness: 8–9/10 depending on consistency
Estimated cost: $80–150/session (may be lower with subscription plans)
At-home Devices: Foot Massagers with Heat
Brands: RENPHO, Miko Shiatsu, Belmint
How it works: Combine compression, vibration, and heat to relax soft tissue and improve blood flow. Picture it like a warm-up routine for tired, tense joints.
How to use: 15–30 minutes daily after work or before bed
Effectiveness: 6–7/10 for symptom relief
Estimated cost: $100–180 (approx. €90–170)
Recommended by: Reyus Mammadli, medical consultant: “They’re a smart, low-cost way to reduce nighttime swelling and increase circulation before bed.”
Injectable Biologics and Advanced Therapies
Examples: Corticosteroid injections, Platelet-Rich Plasma (PRP)
How they work: Corticosteroids reduce inflammation instantly, while PRP (derived from your own blood) stimulates tissue healing. These options aim not just to relieve pain but also to slow or reverse joint degeneration.
How they’re administered: Done in a clinical setting; 1–3 injections per site spaced weeks apart.
Effectiveness: 8–9/10 depending on diagnosis and technique
Estimated cost: Corticosteroids: $100–250/injection; PRP: $500–1,200/session (approx. €90–1,100)
Best for: Moderate to severe arthritis or tendon-related damage not responsive to basic care.
Newer technologies like wearable vibration therapy devices (e.g., Therabody JetBoots) are also gaining traction for managing stubborn inflammation and enhancing recovery ⧉.
When Should You Worry?
Here’s when you shouldn’t just shrug it off—and more importantly, why:
- Pain lasts more than 2 weeks: Occasional soreness is normal after overuse, but if pain persists beyond two weeks—even if it comes and goes—your body is signaling an underlying issue. Lingering inflammation could point to early arthritis, tendon strain, or nerve compression that won’t resolve on its own.
- Joints appear visibly deformed: This isn’t just cosmetic. Visible deformities—like bony protrusions, misalignments, or swollen joints—often indicate progressive joint deterioration. If one foot starts looking noticeably different from the other, especially at rest, it’s time to act.
- You experience fever or fatigue with the pain: These are red flags for systemic inflammation or infection, such as rheumatoid arthritis, gout flares, or even early cellulitis. If the foot pain coincides with flu-like symptoms, don’t wait it out—seek medical evaluation.
- The pain worsens rapidly or spreads: If discomfort escalates quickly, spreads to other joints, or starts affecting your gait, it may be a sign of inflammatory or autoimmune processes. For example, foot pain that jumps from one joint to another could signal migrating arthritis or reactive joint inflammation.
Even if symptoms seem intermittent—say, every third evening—their pattern still matters. Pain that returns cyclically is often more concerning than one-off soreness because it hints at a chronic condition silently progressing.
Chronic joint pain could signal progressive conditions like rheumatoid arthritis or even diabetic neuropathy. According to the CDC, over 24% of American adults suffer from diagnosed arthritis ⧉—but many more go undiagnosed for years. According to the CDC, over 24% of American adults suffer from diagnosed arthritis ⧉—but many more go undiagnosed for years.
Can You Prevent It from Happening?
Preventive measures aren’t rocket science—but they work. Let’s break down how each one can help, and what to expect:
- Switching to shock-absorbing shoes with arch support: Good footwear helps redistribute pressure evenly across the foot and reduce joint strain. If your current shoes lack support, even short walks can become painful. This simple change is often a game-changer.
- Effectiveness: 8/10
- When it works: Expect improvement within 1–2 weeks of daily use. If pain persists beyond that, look into orthotics.
- Elevating your feet for 15–20 minutes each evening: This encourages venous return and reduces fluid buildup in the lower extremities. It’s especially useful after long periods of standing or sitting.
- Effectiveness: 6/10
- When it works: You may notice reduced swelling and tension within a few days. If there’s no change in a week, it may not be your key method.
- Staying hydrated: Joints need fluid to maintain lubrication. Dehydration contributes to stiffness and makes cartilage more prone to wear. Think of your joints like engine parts—they need oil to run smoothly.
- Effectiveness: 5/10 (but supports other treatments)
- When it works: Subtle but important. Combine with diet and stretching for better results.
- Maintaining a healthy weight: Less weight = less pressure. Every pound you lose can remove 4–6 pounds of force off each foot joint when walking.
- Effectiveness: 9/10 for those who are overweight
- When it works: Expect gradual improvement over weeks. A 5–10% drop in body weight often brings noticeable relief.
- Doing daily foot and calf stretches: These help maintain mobility and reduce tension in tendons and fascia. Flexibility supports proper foot mechanics and minimizes joint friction.
- Effectiveness: 7/10
- When it works: Can bring daily relief after just a few sessions. Best used long-term.
A practical trick? Freeze a water bottle and roll it under your arch for 10 minutes after work. Cheap, easy, and oddly satisfying.
What About Natural or Home Remedies?
While we’re not getting into herbs and incense, some well-supported home methods can genuinely reduce discomfort—if used correctly and consistently. Here’s a closer look at the most effective ones:
Warm Epsom Salt Soaks
What it does: Magnesium sulfate helps reduce inflammation and ease joint stiffness.
How to use: Dissolve 1/2 cup (120 g) of Epsom salt in a basin of warm water (about 100°F or 38°C). Soak your feet for 15–20 minutes.
How often: 3–5 times per week.
When to consider stopping: If there’s no improvement after 10 days.
Effectiveness: 6/10.
Estimated cost: ~$5–10 (approx. €4–9) for a large bag.
Contrast Baths (Hydrotherapy)
What it does: Alternating hot and cold water improves circulation and helps reduce inflammation. Think of it as interval training for your blood vessels.
How to use: Soak feet in hot water (100–104°F / 38–40°C) for 3 minutes, then switch to cold water (50–60°F / 10–15°C) for 1 minute. Repeat 3–4 cycles, always ending with cold.
How often: Once daily during flare-ups.
When to stop: If discomfort increases or skin becomes sensitive.
Effectiveness: 7/10.
Estimated cost: Free with home supplies.
Anti-inflammatory Diet
What it does: Helps reduce systemic inflammation that contributes to joint pain.
How to follow it: Eat 2–3 servings of fatty fish weekly, add nuts, berries, leafy greens, and avoid processed foods and excess sugars.
How long to try it: At least 4–6 weeks to assess effect.
When to stop: If no noticeable changes or gastrointestinal discomfort worsens.
Effectiveness: 6–7/10 depending on consistency.
Estimated cost: $15–40/week extra (approx. €14–38).
Foot Rolling with a Frozen Bottle
What it does: Cold massage that relieves soreness and promotes circulation.
How to use: Freeze a plastic bottle of water. While seated, roll it under the arches of your feet for 10 minutes.
How often: Daily after long periods of standing or walking.
When to stop: If numbness or discomfort develops.
Effectiveness: 5/10 alone; up to 8/10 when used with other methods.
Estimated cost: Free.
Gentle Stretching Before Bed
What it does: Loosens tight muscles and tendons that compress joints. Think of it like uncoiling a spring.
How to do it: Try calf wall stretches and toe flexor stretches—hold each for 30 seconds per leg, repeat 2–3 times.
How often: Every evening.
When to stop: If pain worsens during stretching.
Effectiveness: 7/10.
Estimated cost: Free.
These options are particularly helpful for people in early stages of arthritis or with occasional flare-ups ⧉.
Are Certain People More at Risk?
Absolutely. Risk factors include:
- Age 45 and older: As we age, cartilage in joints naturally wears down and the body’s ability to regenerate it decreases. Think of it like the tread on your favorite pair of sneakers—eventually, it thins out. Older adults also tend to have slower circulation and more chronic inflammation, both of which can intensify foot pain by day’s end.
- High-impact jobs (retail, healthcare, manufacturing): These professions often require long hours of standing or walking on hard surfaces, which loads constant pressure onto the foot joints. Imagine jumping up and down on a trampoline all day—except the trampoline is concrete. The repetitive microtrauma builds up and flares more intensely in the evening when the muscles and joints are fatigued.
- Obesity (BMI >30): Extra weight acts like carrying a backpack of bricks all day long. Every additional pound increases the pressure on your foot joints severalfold. That mechanical overload wears down joint surfaces, triggers inflammation, and causes evening pain as the weight has been pressing all day.
- Family history of joint diseases: Genetics often determine how resilient or vulnerable your joints are. If joint issues run in your family, you may inherit biochemical traits (like poor collagen integrity or excessive inflammatory responses) that predispose you to pain. It’s like inheriting the same faulty wiring—eventually, the circuit shorts out.
- Wearing unsupportive footwear like flip-flops or high heels: Fashion often fails function. Shoes without proper arch support or cushioning redistribute pressure unevenly, straining ligaments and joints. Picture walking barefoot on cobblestones for 10 hours—it adds up. Even minor misalignments, when repeated daily, can lead to significant evening pain.
A male nurse in his 30s from Houston, Texas, developed nightly foot joint pain after transitioning to 12-hour shifts. Simply upgrading to gel-cushioned clogs and adding a nightly stretching routine made a world of difference. Simply upgrading to gel-cushioned clogs and adding a nightly stretching routine made a world of difference.
Editorial Advice
Reyus Mammadli, medical consultant, emphasizes: “Most evening foot joint pain is preventable or manageable with the right habits and diagnostics. Ignoring it will only make things worse.”
He also advises patients not to over-rely on over-the-counter pain relievers: “They mask symptoms but don’t fix root problems. You need diagnostics and a treatment plan tailored to your case.”
When in doubt, book a visit to a podiatrist or a rheumatologist. Early intervention can prevent permanent joint damage. And hey—your feet carry you through life. Don’t they deserve a little evening TLC?
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.