The operating room is a hub of complex medical procedures that are both frightening and inspiring. One of these is intubation during surgery, an often underestimated procedure that plays an important role in every major operation.
Purpose
Intubation during surgery, simply put, involves the insertion of a flexible plastic tube into the trachea. This life-saving step helps establish a safe and secured airway, intending to support the patient’s breathing while under anesthesia. The tube serves as the gateway for ensuring the smooth flow of oxygen and anesthetic gases into the lungs, and removing carbon dioxide.
Role of intubation in maintaining patient airway and ventilation
From the medical practitioner’s point of view, the process of intubation is akin to an art form in itself. It ensures the patient’s airways remain open and properly ventilated regardless of the surgical position. A challenge they often face is dealing with drooling or possible regurgitation caused by anesthesia. Hence, intubation provides a protective barrier that prevents aspiration, thus securing the patient’s breathing throughout the operation. It’s this meticulous attention to detail that allows surgeons to carry out complex procedures with the utmost confidence.
Types of Intubation Techniques
Any medical practitioner knows that surgical procedures often require specific approaches to ensure patients’ comfort and safety. One such technique is intubation, strategically performed applying either orotracheal or nasotracheal methods depending on the surgery type and patient’s situation.
Orotracheal intubation
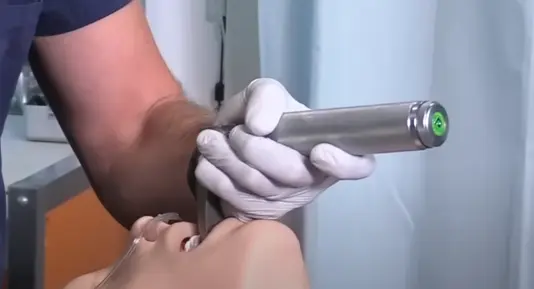
Orotracheal intubation is abundantly practiced due to its simplicity and effectiveness. In this procedure, a tube is inserted through the mouth into the windpipe, ensuring the airway remains clear during surgery. But attention should be given not to cause any injury to the patient’s teeth or mouth tissues during the process.
Nasotracheal intubation
Nasotracheal intubation, although less common, is a useful alternative in select cases, especially for oral surgeries. The tube is placed into the nose and then down the trachea. While it provides a clear access point, care should be taken to avoid complications like nosebleeds or sinusitis.
In conclusion, both methods have their benefits and drawbacks, making the choice highly dependent on the surgical procedure, patient’s health condition, and the healthcare provider’s experience. But nonetheless, proper application of either technique realizes a significant role in the patient’s comfort and surgical success.
The Procedure of Intubation
Intubation during surgery is an essential procedure that ensures a patient’s airway remains open, stable, and oxygenated. The process involves a meticulous approach to ensure patient safety and successful outcomes.
Preparing the patient and the operating room
The preparation phase is crucial as it determines the overall success of the intubation process. Checking the patient’s airway anatomy, the appropriate functioning of the equipment, and the sterilization of the operating room forms the basis of the procedure.
Step-by-step process of intubation
The process begins with the insertion of an endotracheal tube in the patient’s airway, followed by confirmation using a digital sensor and auscultation to affirm successful placement. Adjustments are made swiftly if any complications arise to safeguard the patient’s wellbeing. It remains a distinguishing aspect of surgical cases, highlighting the seamless blend of skill, precision, and medical knowledge.
Potential Complications and Risks
When undergoing a surgical procedure, it’s possible that a patient will be intubated. This is a routine process that provides a secure airway for the administration of anesthetics or ventilatory support. However, it’s essential to be mindful of potential complications associated with the procedure.
Minor issues, such as a sore throat, oral or dental injuries or nausea, may occur. More severe cases may include aspiration pneumonia, barotrauma and the extremely rare but potentially fatal anoxia.
Experienced clinicians who understand the inherent risks and follow strict procedural guidelines can significantly minimize these hazards. Proper skill and technique, coupled with vigilant monitoring can help ensure a safer intubation process during surgery. It is a critical part of perioperative care, making it crucial that the clinicians involved are well-versed in its execution.
Alternative Airway Management Techniques
Managing the airway of a patient during surgical procedures is absolutely crucial and requires a high degree of precision and knowledge. Various techniques and devices exist for airway management, two of which are supraglottic airway devices and transtracheal catheterization.
Supraglottic Airway Devices
Supraglottic airway devices, a favored choice for many anesthesiologists, offer distinct advantages. They are easy to insert, require less patient manipulation, provide reliable conduits for ventilation, and significantly reduce the risk of trauma compared to endotracheal intubation.
Transtracheal Catheterization
Transtracheal catheterization, another alternative, is primarily used in emergencies when other techniques fail to secure the airway. It’s a minimally invasive method, but medical professionals must be mindful of potential complications such as infection and the risk of misplacement.
Recovery and Post-Intubation Care
During surgical procedures, especially when under general anesthesia, intubation is often necessary. It involves placing a tube into a patient’s windpipe (trachea) to maintain an open airway, aid in breathing, or administer certain drugs. However, post-surgery, extubation — the removal of the tube — and monitoring for complications are equally as critical.
Extubation process and considerations
Once surgery is completed, and the patient shows signs of waking up, the medical team begins the careful process of extubation. Here, timing is crucial. Extubating too early can lead to breathing problems or the need to re-intubate. Conversely, delaying extubation could expose the patient to possible complications like infections.
Monitoring and managing complications post-intubation
The care team remains vigilant, closely monitoring the patient for signs of post-intubation complications, including pain, hoarseness, or difficulty swallowing. In more severe cases, damage to the trachea or vocal cords may occur. Physicians ensure that any discomfort or complications are swiftly, effectively managed to pave the way for a successful recovery.
Conclusion
When it comes to surgical procedures, intubation undeniably plays a crucial role. It not only facilitates the provision of anesthesia but also maintains patient’s airways open.
Proficiency in Intubation: An integral part of surgeries, intubation, if performed improperly, could lead to serious complications, including damage to the throat or trachea. It emphasizes the importance of a well-executed methodology. With the right technical skills and knowledge, medical professionals mitigate the potential risks linked to the process.
Patient Safety: The primary aim of medical procedures is preserving patient safety with the highest regard. Thus, the proper use of intubation techniques guarantees the maintenance of this safety precedence, ensuring a secure surgical environment for patients and clinicians alike. The positive implication of this seamless procedure reflects directly on the patient’s recovery and overall surgical outcome. Therefore, mastery in intubation techniques is a vital box to check in the surgical safety checklist.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.