Knee arthritis has another more common name among medical professionals – gonitis. The disease can be defined by a typical clinical picture, quite pronounced symptoms of musculoskeletal lesions.
The inflammatory process in the tissues that form the joint has different causes, so sometimes the treatment of arthritis of the knee joint can be a simultaneous task for several related doctors.
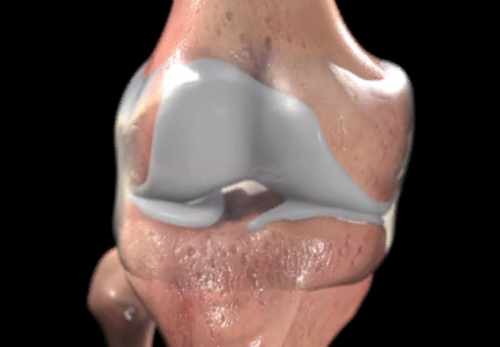
Structure of the Knee
The knee is a complex element of the musculoskeletal system, which provides flexion, extension movements of the lower limb in this department. The articulation is based on the following bony components:
- The distal portion of the femur (inner, outer condyle);
- Proximal part of the tibia (also inner, outer condyle, tibial plateau);
- The patella is a flat bone, which is surrounded on all sides by connective tissue fibers of the tendon coming from the thigh muscles (easily palpable through the skin on the anterior surface of the articulation).
The articular bony surfaces of the femur and tibia are not compatible, and there is a cartilage layer between them for normal gliding. The cartilage in the knee takes the form of paired formations – menisci. The menisci are horseshoe-shaped (convexly facing outward) and are anatomically distinguished:
- The body (the most massive part);
- The anterior horns;
- Posterior horns.
An important role in the knee is played by the tendon-ligament apparatus, which ensures the stability of the articulation in the sagittal, frontal planes. Posterior and anterior cruciate ligaments prevent pathological anteroposterior motion. If they are torn, the “drawer” symptom appears, when with the tibia fixed, the femur can be displaced backward. To fight the disease, it is necessary to know exactly the symptoms and treatment of arthritis of the knee.
The medial and lateral collateral ligaments provide immobility to the knee in relation to the outside and inside. If the inner or outer collateral ligaments are torn, a valgus (toward the midline) or varus (away from the midline) deformity of the lower extremity can occur.
Causes of Knee Arthritis
Only infection can be the cause of knee arthritis. There is unequivocally some truth to this statement, but despite the overwhelming number of bacterial, there are other factors that lead to knee damage.
Infectious arthritis can result from the introduction of the following pathogenic agents into the joint cavity and synovial membrane:
- Bacteria (causative agents are gram-positive, gram-negative microbes, and infection (such as tuberculosis) is also possible);
- Viruses (viral infection is little specific for joint lesions, but we should not forget about this group of pathogens);
- Fungi (actinomycosis, candida);
- Microparasites (schistomatosis, echinococcosis, opisthorchiasis and others).
Knee arthritis can also occur due to the following damaging factors:
- Compression overload of the knee (repetition of the same type of movements when jumping and running);
- Unequal distribution of body weight on the knee (can occur with spinal deformities such as severe scoliosis or kyphosis of the lumbar and thoracic regions). Constant overloading of other joints of this limb with gradual development of arthrosis of the hip and ankle joints can also occur;
- Prolonged exposure to positions which result in local overpressure on the articular cartilage (positions with a focus on the knees);
- Prolonged exposure and localized exposure of the knee area to low temperatures. Exposure to extreme environmental conditions is not necessary, regular draughts are sufficient;
- Traumatic damage to the soft tissues in the knee: menisci, ligaments, subchondral tissue and joint capsule (aseptic inflammation develops);
- Age-related changes (with age, the cartilage layer becomes thin, so the knee can no longer adequately perform its cushioning and protective functions);
- A person’s tendency to have allergic reactions (with sensitization, there is a probability of developing reactions from the synovial lining as well);
- In the presence of somatic diseases, the likelihood of reactive inflammation in the knee cavity increases. Gonitis can occur against the background of pleuropneumonia, scurvy, scarlet fever, sarcoidosis, systemic collagenosis, blood cancers, systemic lupus erythematosus, scleroderma, vasculitis, and many others.
There is a possibility of involvement of the knee in the inflammatory process even in the presence of a sexually transmitted infection. Such a condition is called Reiter’s syndrome. Such patients have urethritis (inflammation of the urethra) and conjunctivitis (inflammation of the conjunctiva of the eye).
We should also not forget about the factor of genetic predisposition, which determines the functional, morphological features of tissues or structures of the knee. It has been proven that due to heredity, underdevelopment of the menisci or ligaments of the articulation is possible. Under poor conditions, these structural features can lead to the gradual development of a cascade of pathogenetic reactions. However, if a person is not exposed to the action of provoking external as well as internal factors, there will be no conditions for the emergence of the disease.
Classification of Knee Arthritis
According to the course of the pathological reactive process, the following types of knee joint arthritis are distinguished:
- Primary, when the focus of pathogen development was originally located in the synovial lining tissues of the knee joint. There are no similar foci of inflammation or background diseases that may have contributed to the gonitis in the body.
- Secondary knee arthritis (reactive) is an inflammatory response of the articular tissues in response to the presence of a related disease. It involves cartilage and synovial elements during pathogenesis. Triggers are systemic autoimmune processes, rheumatic reactions, skin diseases (psoriasis). Secondary arthritis can develop against a background of decreased tissue density of adjacent bones.
There are these main varieties of primary gonitis:
- Essential (idiopathic) arthritis – a form of the disease in which it is impossible to determine the primary source of the pathology. To make such a diagnosis, it is necessary to perform all investigations that exclude another character of inflammation;
- Posttraumatic arthritis of the knee (when collecting the anamnesis data, a direct connection of gonarthritis with a traumatic impact on the knee area is revealed);
- Infective arthritis of the knee (with primary tissue damage from bacteria, viruses, or fungi);
- Rheumatoid arthritis of the knee joint (the final etiology and pathogenesis of rheumatoid gonitis have not yet been established, but the role in the development of the pathology is attributed to autoimmune processes).
Secondary arthritis is subdivided according to the underlying disease that led to the joint pathology (psoriatic, reactive, osteoarthritic and others).
Knee Arthritis Symptoms
Most clinical cases reveal an acute course of gonarthritis. The disease most often occurs abruptly. In the case of essential arthritis, the appearance of inflammation is not preceded by anything. In other cases, a connection is established with trauma, sports load or concomitant diseases.
The course of the disease is characterized by the following symptom complex:
- Swelling of the soft tissues around, as well as an increase in its size (the appearance of asymmetry is possible);
- A pronounced pain syndrome (and the pain can bother both at rest and when moving the limb);
- Local hyperthermia of the skin above the knee (due to full blood vessels in the inflammation focus);
- Restriction of knee mobility due to pain and swelling (after a course of therapy of knee arthritis, mobility is fully restored);
- Impairment of normal gait (due to inability to fully bend the leg);
- Intoxication of the body (increased body temperature, weakness, headaches).
Diagnosis
If a patient has phenomena of knee lesions, the traumatologist first of all conducts an objective examination. After examination, palpation and auscultation of the joint, the doctor makes a preliminary diagnosis and determines what additional methods of examination may be necessary.
To rule out the presence of fluid or blood in the joint cavity, an ultrasound examination is prescribed. X-rays may be needed to assess the condition of the adjacent bones. It may reveal a fracture, dislocation, narrowing of the cartilage gap, or the presence of osteophytes (bone growths). If a more thorough assessment of the condition of the bone tissues is necessary, a CT scan is prescribed.
For differential diagnosis with meniscus and ligament apparatus injuries, magnetic resonance imaging is prescribed, which allows good visualization of soft tissue formations.
Sometimes doctors perform punctures of the joint (in the presence of exudate in its cavity). The extracted synovial fluid is sent for laboratory examination (microscopic, bacteriological, and biochemical studies are performed). In addition, during the manipulation of the possible introduction of drugs directly into the joint cavity. Without using all diagnostic methods, the treatment of knee arthritis will be ineffective.
Knee Arthritis Treatment
Treatment with conservative methods
Treatment of arthritis of the knee joint is a combination of medication and local therapy. In the development of secondary gonarthritis, along with the treatment of joint pathology, it is necessary to carry out therapeutic measures for the underlying disease.
In addition to drug treatment, attention should be paid to such measures as the normalization of body weight (to reduce the load on the knees), a rational diet, exercise therapy. Physical therapy procedures (ultrasound, mud and ozokeritic wraps, therapeutic baths, warming) show a good effect in the treatment of arthritis of the knee joint.
When drawing up a treatment regimen, the etiological factor and symptoms of the disease are taken into account.
With infectious sources of inflammation, it is advisable to prescribe the appropriate groups of drugs (antibacterial, antifungal and antiviral).
Treatment of arthritis of the knee joint includes the following groups of drugs:
- Anti-inflammatory (with a mild and moderate course, non-steroidal, and with severe – steroidal (glucocorticosteroids) medications are used);
- Analgesic (both oral and ointmental forms can be used);
- Metabolic (improving regeneration processes in cartilage tissues);
- Immunomodulatory (to improve the body’s resistance);
- Vitamin remedies.
There are good effects in the local treatment of arthritis of the knee joint (compresses, ointments, gels, lotions, emulsions).
Single and daily dosages of drugs, the duration of the course of treatment of arthritis of the knee joint is determined by the attending physician. He takes into account the etiology, the severity of the disease, as well as the individual characteristics of the patient’s body. If there is intolerance to the medication, this should be immediately reported to the doctor to address the issue of the possibility of further use of the drug prescribed or the selection of a suitable analogue.
It is worth noting that conservative methods of treatment of knee arthritis achieve results, however, are not entirely comfortable for the patient. In addition, standard therapeutic measures do not give a 100% guarantee of getting rid of the disease. Doctors now recommend the MBST method of therapy, because it can replace other treatment methods and restore the joint the fastest.
Treatment of knee arthritis with MBST therapy
Specialists in the field of joint arthritis treatment offer the most effective treatment for arthritis of the knee joint – MBST-therapy. It is a unique non-invasive method, which significantly enhances the regeneration of affected tissues by blocking the synthesis of inflammatory mediators, suppressing anaerobic cycles and supporting hemostasis within cells.
As a result, it is possible to stop the pain syndrome, relieve restrictions in mobility, improve tissue trophism and in general make the treatment of knee arthritis more qualitative and effective. It is noteworthy that after MBST treatments, tissue buildup is noted over the course of a year.
MBST therapy does not cause any adverse reactions and does not harm other body systems. To restore bone and cartilage tissues it will be enough to undergo several procedures (usually 5-9 times is enough), taking only 1 hour a day.
If you want to restore mobility to your knee, relieve pain and improve your quality of life, you should make an appointment by phone in advance for an initial consultation. Your doctor will choose for you an individual program, which will take place on the treatment of arthritis of the knee. And just a few weeks later you will be able to return to a full life and forget about the pain forever!
People who are overweight should be recommended to limit the consumption of animal fats and simple carbohydrates in order to reduce body weight.
The intake of table salt and spices should be limited. The diet should be enriched with foods containing large amounts of vitamins and fiber (fresh fruits and vegetables). It is recommended to enrich the diet with healthy fats, which are very useful for joints (nuts, avocados, vegetable seeds, sea fish and seafood).