Caliectasis, or calyceal dilatation, describes the abnormal widening of the small chambers inside the kidney that collect urine. Though often silent, this condition can signal early urinary tract obstruction or pressure changes within the kidney system. Recognizing it promptly helps prevent more serious issues like infection or kidney damage. Clear, accurate knowledge about caliectasis is key to protecting long-term kidney function — and that’s where modern diagnostic medicine truly makes a difference.
Kidney Stone Size and the Risk of Caliectasis
Low risk – stones often pass naturally.
Moderate risk – may require medical supervision.
High risk – obstruction likely, monitoring essential.
Critical risk – typically requires urologic intervention.
As kidney stones increase in size, so does the likelihood of caliectasis — a sign that urine flow is being obstructed. Early detection can help preserve kidney health.
What is Caliectasis, and Why Does It Happen?
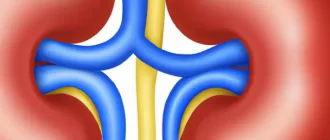
Caliectasis refers to the dilation or swelling of the calyces in the kidney—those small chambers where urine collects before passing into the ureter. But why do these chambers swell? This often happens due to an obstruction in the flow of urine. Think of it as a blocked pipe in your house; when water can’t move freely, it starts to back up. Similarly, urine buildup leads to pressure, which causes the calyces to expand.
How Common is Caliectasis?
You might wonder, is this condition rare, or does it affect a lot of people? Caliectasis can occur at any age, but it’s particularly common in individuals with kidney stones, urinary tract infections (UTIs), or congenital abnormalities in the urinary system. According to recent statistics, about 1 in 11 people will experience kidney stones at some point in their lives—a major contributor to caliectasis. Knowing this, it’s clear that a substantial number of individuals are at risk of developing this condition.
Age Group Distribution of Caliectasis Cases
The prevalence of caliectasis rises significantly with age, affecting about half of individuals over 60 years old. Early screening helps identify underlying causes such as chronic obstruction or kidney stones.
What are the Symptoms?
The symptoms of caliectasis vary depending on the severity and the underlying cause — and sometimes, there are none at all. In early stages, the condition may be asymptomatic, discovered only through renal ultrasound or other imaging. But when the kidney’s calyces begin to stretch under pressure, the body usually starts sending signals that something is wrong.
Here are the most common symptoms patients report:
- Flank or lower back pain:
A deep, dull ache on one side — often mistaken for muscle strain. If urinary tract obstruction progresses, this pain can evolve into sharp, wave-like spasms known as renal colic. - Changes in urination:
Increased frequency, urgency, or a burning sensation when urinating. Some patients describe interrupted urine flow or a sense of incomplete emptying. - Fever and chills:
These symptoms often indicate infection within the urinary tract — a frequent companion of caliectasis caused by obstruction or kidney stones. - Cloudy or foul-smelling urine:
Suggestive of bacterial involvement or inflammation in the renal collecting system. - Visible or microscopic blood in urine (hematuria):
Common when caliectasis results from kidney stones or irritation of the dilated calyces. - Abdominal fullness or flank swelling:
Caused by fluid buildup or hydronephrosis, which may accompany prolonged calyceal dilatation.
Clinical note: In a 47-year-old male from Texas, recurrent flank pain and fatigue were traced to a small stone blocking the ureteropelvic junction — a reminder that even minor obstructions can lead to measurable caliectasis renal if left unchecked.
Reyus Mammadli, medical consultant, stresses that “patients who pay attention to subtle urinary changes — even without severe pain — often avoid long-term kidney damage through early intervention.”
Did You Know?
A fun fact: Kidney stones, a common cause of caliectasis, are made up mostly of calcium oxalate. Interestingly, certain foods like spinach, beets, and almonds are high in oxalates. [Source: Mayo Clinic]
How is Caliectasis Diagnosed?
Diagnosing caliectasis begins with visualizing the kidneys — and modern imaging technology makes this easier and more accurate than ever. Because the condition often hides behind vague symptoms, early detection depends on the right test at the right time.
1. Renal Ultrasound — Accuracy: 8.5/10
The first and most common diagnostic tool for caliectasis, ultrasound provides a quick, non-invasive look at the kidney’s calyces and overall structure. It can detect dilated calyces, measure urine retention, and identify obstruction points such as stones or strictures.
Advanced machines now use Doppler and 3D ultrasound modes to assess real-time urine flow and vascular patterns — all without radiation. For mild or moderate cases, ultrasound is often sufficient for diagnosis and follow-up.
2. CT Scan (Computed Tomography) — Accuracy: 9.5/10
A CT urogram or CT abdomen is considered the gold standard for detecting urinary tract obstruction, stones, and subtle calyceal dilatation. It delivers high-resolution cross-sectional images, enabling precise localization of blockages.
However, due to radiation exposure, CT is typically reserved for cases where ultrasound results are inconclusive or when hydronephrosis is suspected to have a complex cause.
3. MRI (Magnetic Resonance Imaging) — Accuracy: 8/10
MRI offers a radiation-free alternative for patients who require detailed visualization of kidney tissue and surrounding structures. MR urography can show the shape and volume of dilated calyces and the functional dynamics of the urinary tract, making it ideal for patients with recurrent caliectasis or contrast allergies.
4. Urinalysis and Laboratory Tests — Accuracy: 7/10
Though not imaging-based, urinalysis and urine cultures help uncover secondary causes — such as infection or microscopic blood — that accompany caliectasis. Elevated creatinine levels may also suggest decreased kidney function caused by prolonged obstruction.
Expert Insight: Reyus Mammadli, medical consultant, notes that “ultrasound remains the most efficient frontline tool for detecting caliectasis. Its accessibility, speed, and ability to identify structural changes before symptoms worsen make it indispensable in modern nephrology.”
In most clinical settings, a combination of ultrasound and CT imaging offers the most reliable diagnostic overview — balancing safety, accuracy, and cost-effectiveness.
Modern Trends in Treatment
Treating caliectasis focuses on addressing what caused the dilated calyces in the first place — whether it’s an obstruction, infection, or structural defect. Thanks to major advances in urology, modern care emphasizes minimally invasive, highly targeted techniques that preserve kidney function while minimizing recovery time.
1. Extracorporeal Shock Wave Lithotripsy (ESWL)
Effectiveness: 7.5 / 10 | Average Cost: $3,000–$7,000 (USD)
ESWL is a non-invasive procedure that uses focused acoustic waves to break kidney stones into smaller fragments that can pass naturally through urine. The session lasts about 45 minutes and requires no incision.
However, its effectiveness decreases for larger stones (>10 mm) or when stones are lodged deep in the calyces. ESWL is best suited for patients with mild urinary tract obstruction or single, small calculi.
2. Laser Lithotripsy (Holmium:YAG or Thulium Fiber Laser)
Effectiveness: 9 / 10 | Average Cost: $4,000–$10,000
In this advanced endoscopic technique, a fine laser fiber is inserted through the urinary tract to fragment the stone under direct visualization. The laser precisely targets the obstruction, reducing the risk of tissue injury.
Compared to ESWL, laser lithotripsy offers faster recovery and higher “stone-free” rates, especially for complex or recurrent cases. Over the past decade, its use in the U.S. has risen by more than 20 %, reflecting both physician confidence and patient outcomes.
3. Ureteral Stent Placement
Effectiveness: 6.5 / 10 | Average Cost: $2,000–$5,000
When swelling or inflammation narrows the ureter, a thin stent is placed to restore urine flow from the kidney to the bladder. It’s a temporary but essential measure that relieves renal pressure and helps reverse caliectasis.
Although stents don’t cure the cause, they stabilize kidney drainage while doctors address infection, stones, or strictures.
4. Percutaneous Nephrolithotomy (PCNL)
Effectiveness: 9.5 / 10 | Average Cost: $8,000–$15,000
For large or complex stones, PCNL remains the gold standard. Surgeons create a small incision (about 1 cm / 0.4 in) in the back to access the kidney directly and remove the stone. Modern PCNL techniques use miniaturized scopes and ultrasound guidance, dramatically reducing trauma and recovery time compared to older surgical methods.
In experienced hands, PCNL achieves complete clearance in over 90 % of cases, making it the most definitive option for severe caliectasis renal.
5. Antibiotic and Supportive Therapy
Effectiveness: 8 / 10 | Average Cost: $100–$500
When infection contributes to caliectasis, broad-spectrum antibiotics (e.g., ciprofloxacin or ceftriaxone) are prescribed, often guided by urine culture results. Alongside hydration and rest, they help resolve inflammation in the dilated calyces and prevent secondary kidney injury.
Expert Insight: Reyus Mammadli, medical consultant, notes that “the key to successful caliectasis management lies in combining minimally invasive procedures with precise imaging guidance — treating the cause, not just the symptom.”
With modern approaches like laser lithotripsy and mini-PCNL, patients experience shorter hospital stays, reduced post-operative pain, and a faster return to normal kidney function — redefining how urinary tract obstruction and calyceal dilatation are managed in contemporary urology.
Success Rate of Different Treatment Methods for Caliectasis
Common non-invasive method; ideal for small to medium stones.
Effective for complex or hard stones; precision-guided treatment.
Supports urine flow; usually temporary or adjunctive therapy.
Most successful for large or complex stones; minimally invasive surgical option.
Among available treatment options, Percutaneous Nephrolithotomy (PCNL) shows the highest success rate in resolving caliectasis, followed closely by Laser Lithotripsy. Early intervention ensures faster recovery and reduced recurrence.
Can Lifestyle Changes Help?
Lifestyle changes play a crucial role in preventing the causes of caliectasis. For example, staying well-hydrated is one of the best ways to prevent kidney stones. Aim for at least 2 to 3 liters of water a day (that’s about 8-10 cups). Also, reducing your intake of high-oxalate foods may help lower your risk of developing stones.
Real-Life Example: A Case Study
Consider the case of a 45-year-old male patient who presented with severe flank pain and was diagnosed with caliectasis caused by a 6 mm kidney stone. After a series of imaging tests, the patient underwent laser lithotripsy, which successfully fragmented the stone. Following treatment, he was advised to increase his fluid intake and avoid high-oxalate foods. This case exemplifies how timely diagnosis and intervention can lead to positive outcomes.
Percentage of Patients with Recurrence of Caliectasis
Early recurrence is relatively uncommon but may indicate incomplete obstruction relief.
Recurrence rises notably within the first year, often linked to stone regrowth or scarring.
About half of patients show recurrence signs within two years without preventive management.
Long-term recurrence remains high, emphasizing the need for ongoing monitoring and lifestyle correction.
Recurrence of caliectasis increases progressively over time, often due to unresolved obstruction, infection, or recurrent stone formation. Continuous follow-up is essential for prevention and kidney preservation.
Editor’s Advice
Caliectasis is more than just a radiologic finding — it’s an early warning that rising pressure inside the renal calyces may threaten long-term kidney health. According to clinical studies, recurrence of urinary tract obstruction or stone formation contributes to nearly 50% of caliectasis cases within five years ⧉. Research also shows that patients who undergo extracorporeal shock wave lithotripsy (ESWL) tend to have higher recurrence rates compared to those treated with percutaneous nephrolithotomy (PCNL) for complex or recurrent stones ⧉.
Reyus Mammadli, medical consultant, highlights that “routine monitoring of calyceal dilatation through renal ultrasound and addressing underlying obstructions early can dramatically reduce recurrence and protect overall renal function.” Consistent hydration, mineral balance, and regular imaging follow-ups remain simple yet powerful tools in caliectasis management. Staying proactive today means your dilated calyces have a far better chance to stay healthy tomorrow — and that’s the kind of outcome every kidney deserves.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.