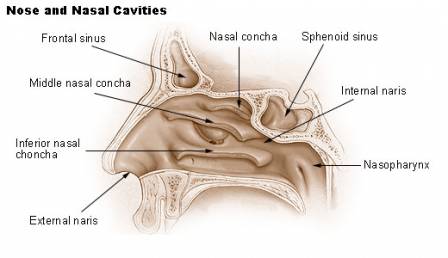
Nasal herpes is a viral condition caused by the herpes simplex virus, leading to small, painful blisters or sores that appear on or just inside the nose. It can feel much like a cold sore in an unexpected place, flaring up suddenly and causing discomfort during everyday actions like breathing or touching the area. Although it often looks minor, this nasal symptom reflects an active viral process beneath the surface.
When herpes affects the nasal area, rather than the lips or mouth, it still follows familiar patterns of viral reactivation. Studies suggest that a large majority of adults carry herpes simplex virus type 1, and outbreaks are more likely during periods of stress, illness, fatigue, or weakened immunity. While some people experience rare episodes, others may notice recurring nasal sores that come and go over time.
U.S. HSV‑1 Seroprevalence by Age Group (14–49)
This chart highlights the increasing trend of HSV‑1 seroprevalence with age among individuals aged 14–49 in the U.S. The data shows a clear pattern: older age groups have significantly higher HSV‑1 rates, underscoring the cumulative exposure over time
If irritation, scabbing, or repeated sores develop inside the nose, understanding nasal herpes helps bring clarity to what’s happening and why. Looking closely at how this condition develops, what triggers flare-ups, and how symptoms can be managed allows the problem to be addressed calmly and effectively. A clear explanation of causes, signs, and options makes it easier to know what steps to take next.
Common Triggers for HSV‑1 Reactivation (%)
This chart presents common triggers that may lead to HSV‑1 reactivation. Stress is the leading factor, followed by fever or general illness, and then sun or UV exposure. Understanding these can help individuals better manage their condition.
What are the symptoms of herpes on the nose?
Recognizing nasal herpes can be tricky, especially since its early signs mimic other common conditions. Understanding the symptom profile helps distinguish it from acne, allergic reactions, or even minor skin infections.
- Tingling, itching, or burning: This is often the first and most telling sign—think of it as the ‘red flag’ for an oncoming outbreak. It’s usually localized and occurs before any visible blisters form. Unlike general itchiness or dryness, this sensation tends to be persistent and sharp, often described as “electric” or “nerve-like.”
- Painful blisters on or inside the nostrils: This is the hallmark of nasal herpes. These blisters are small, grouped, fluid-filled, and tender to touch. Once they burst, they leave behind ulcers that scab over. Unlike pimples or blackheads, these sores hurt—especially when blowing your nose or touching the area.
- Swelling and redness: Inflammation usually accompanies blister formation. It may appear as a subtle puffiness around the nostrils or a more pronounced redness. The difference from other conditions like rosacea or allergies lies in the timing—this follows the blistering, not precedes it.
- Mild fever or fatigue: Some individuals, especially during their first outbreak, may experience systemic symptoms like low-grade fever, fatigue, or general malaise. These are secondary symptoms and usually resolve within a few days, but they’re a strong clue when paired with the other signs.
- Recurring nature: Perhaps the biggest giveaway—nasal herpes doesn’t just come and go once. If you’ve noticed similar symptoms in the same area more than once, with weeks or months between episodes, herpes is a likely culprit.
If you’re experiencing these symptoms in tandem, particularly with a pattern of recurrence, it’s time to consider a proper diagnosis and management plan.
Stages of Nasal Herpes: Step by Step
A light burning or tingling sensation appears around or inside the nose—this is your early warning.
The area becomes red, swollen, and sensitive as the immune system kicks in.
Small, fluid-filled blisters appear, grouped together and often painful to the touch.
The blisters burst and begin to weep, leaving behind shallow open sores.
Sores dry out, forming yellowish-brown scabs as healing begins.
Scabs fall off naturally, leaving smooth skin. Full recovery usually takes 7–14 days.
Source: iythealth.com
Is it contagious?
Oh, absolutely. HSV-1 is highly contagious, especially when blisters are present. It can be spread through skin-to-skin contact, shared personal items like towels, or even through droplets if someone sneezes and has an active sore.
Pro tip: Don’t share razors, lip balm, or towels, especially if someone has visible cold sores.
Who is at risk for nasal herpes?
Anyone can get nasal herpes, but certain groups face higher risks due to behavior, health status, or environmental exposure. Let’s break it down:
- People with a history of oral herpes: If you’ve had cold sores in the past, the HSV-1 virus is already in your system. It can reactivate and spread to other areas like the nose, especially if you touch a cold sore and then rub or scratch your nostrils. The proximity of the nose to the lips makes this a common route of self-transmission.
- Individuals with weakened immune systems: People undergoing chemotherapy, living with HIV/AIDS, or taking immunosuppressive medications (like after an organ transplant) are more susceptible to severe and recurrent herpes infections. Their bodies are less able to contain viral reactivation, and nasal outbreaks may be more painful and prolonged.
- Those frequently exposed to close contact: Healthcare workers, parents of young children, and people in crowded living conditions (like college dorms or military barracks) are more likely to come into contact with infected saliva or skin. The more contact you have, the higher your exposure risk—especially if cold sores are present in others.
- Athletes in contact sports: Wrestlers and rugby players, for instance, may face repeated skin-to-skin exposure, sometimes with abrasions that make it easier for HSV-1 to enter. Herpes gladiatorum, a related skin infection, has been well-documented in these groups, and nasal transmission is a possibility.
A real-world case: A 29-year-old male from San Diego, CA, developed painful nasal sores two days after a weekend camping trip with friends. He had shared a water bottle with someone who later disclosed they had a cold sore.
HSV‑1 Seroprevalence in U.S. by Ethnicity
This chart illustrates disparities in HSV‑1 infection rates among ethnic groups in the U.S. Notably, Mexican‑Americans show the highest prevalence, followed by Non‑Hispanic Black and Non‑Hispanic White populations, highlighting significant public health implications.
How is it diagnosed?
Diagnosis usually starts with a visual exam by a healthcare provider. If it’s unclear, they may perform additional tests:
| Diagnostic Method | Description | Accuracy (1–10) | Average Cost (USD) |
|---|---|---|---|
| Viral Culture | Sample from sore is grown in lab | 7 | $100–$250 |
| PCR Test | Detects HSV DNA from swab | 10 | $150–$300 |
| Tzanck Smear | Looks for HSV-infected cells | 5 | $50–$100 |
| Blood Test | Detects antibodies to HSV | 8 | $50–$200 |
Most modern clinics prefer PCR for its high accuracy. ⧉
What are the treatment options?
There’s no cure for HSV-1, but treatments can significantly reduce symptoms and speed up recovery. Here’s a detailed look at the most common approaches:
Antiviral Medications
These are the cornerstone of herpes treatment and include drugs like acyclovir, valacyclovir (Valtrex), and famciclovir.
- How it works: Antivirals stop the virus from replicating, making symptoms milder and outbreaks shorter.
- Duration: Typically taken for 5–10 days during an outbreak; suppressive therapy may be daily long-term.
- Effectiveness: 8/10 in reducing outbreak duration and symptoms.
- Cost: $20–$100 per treatment cycle; generics are more affordable.
- Complexity: Low. Oral tablets taken at home; some may require a prescription renewal for chronic management.
Pain Relievers
Over-the-counter NSAIDs like ibuprofen or acetaminophen are often used to control pain and inflammation.
- How it works: Reduces pain, fever, and swelling associated with blistering.
- Duration: As needed, typically for 2–5 days.
- Effectiveness: 6/10 for symptom relief only.
- Cost: $5–$15 per bottle.
- Complexity: Very low. Readily available and self-administered.
Topical Creams
Docosanol (Abreva) is FDA-approved for HSV-1 cold sores.
- How it works: Applied directly to the lesion, it blocks viral entry into healthy skin cells.
- Duration: Apply five times daily at the first sign of symptoms.
- Effectiveness: 5/10—modestly shortens healing time when used early.
- Cost: Around $15–$25 per tube.
- Complexity: Low. Requires diligence in early application.
Supportive Measures
Using cool compresses, maintaining hydration, and resting can enhance recovery.
- How it works: Eases discomfort and supports immune response.
- Duration: Throughout the duration of the outbreak.
- Effectiveness: 4/10—helps comfort but does not alter viral activity.
- Cost: Minimal.
- Complexity: None. Home-based self-care.
Reyus Mammadli, medical consultant, recommends initiating antiviral therapy at the first sign of recurrence—especially during tingling or burning phases—to prevent full-blown outbreaks. ⧉.
Can nasal herpes be prevented?
Absolutely—though nothing is 100%. Here are top prevention tips:
- Wash hands frequently, especially after touching your face.
- Avoid direct contact with active cold sores.
- Don’t share personal items (lip balm, towels, drinks).
- Manage stress and get enough sleep—yes, your immune system cares!
Can nasal herpes recur?
Unfortunately, yes. Nasal herpes, like all herpes simplex infections, has a sneaky habit—it can go into hiding and then come back. This is because the virus remains dormant in nerve cells and can reactivate at any time.
- Illness or fever: When your immune system is fighting another infection, it’s easier for HSV-1 to break free from its hiding place. A return outbreak might begin with a familiar tingling or burning sensation around the nose, followed by the appearance of blisters in the same area as before.
- Sun exposure: Ultraviolet light can trigger herpes reactivation. A day at the beach without sunscreen might leave you not only sunburned but also dealing with a fresh crop of nose sores. People often notice redness and sensitivity before visible signs appear.
- Stress or fatigue: Emotional or physical stress lowers immunity and is a well-known reactivation trigger. Many patients report outbreaks after sleepless nights, tight deadlines, or travel. The signs may be subtle at first—itchiness, tenderness, or slight swelling—before the full symptoms develop.
If the sores return in the exact same spot, accompanied by tingling or a mild burning sensation, that’s your cue: it’s not just dry skin or a bug bite—it’s probably a herpes recurrence. Recognizing these early signs allows for faster treatment and can shorten the outbreak.
Are there complications?
Most cases of nasal herpes are mild and self-limiting, but certain complications can occur—some of them more serious than others. Understanding these potential issues helps people manage the infection more proactively.
- Secondary bacterial infection: When herpes blisters break, the open skin becomes vulnerable to bacterial invasion. This can result in increased pain, swelling, pus formation, and even cellulitis. In some cases, antibiotics may be needed to treat the secondary infection.
- Spread to eyes (herpes keratitis): If the virus travels from the nose to the eye, it can infect the cornea—a condition known as herpes keratitis. Symptoms include eye pain, redness, tearing, and blurred vision. Without prompt antiviral treatment, it can lead to scarring and vision loss.
- Emotional stress or embarrassment: Recurring nasal outbreaks, especially when visible, can affect self-esteem and social interactions. Patients may feel anxious, ashamed, or isolated, which can further compromise their immune system and increase the likelihood of future outbreaks.
- Herpes encephalitis: This is a rare but life-threatening complication where the virus spreads to the brain. It typically presents with high fever, confusion, seizures, and altered consciousness. Although very rare, this condition requires immediate hospitalization and intensive antiviral therapy. It’s more likely in people with weakened immune systems. ⧉
Editorial Advice
Nasal herpes might not be a cocktail party conversation starter, but it’s real, and more common than many think. Quick action and informed care go a long way in managing it.
Reyus Mammadli, medical consultant, recommends that anyone with frequent outbreaks consider long-term antiviral therapy and keep their immunity in check with healthy habits.
Extra tip: Apply sunscreen on and around your nose if you’re prone to cold sores—UV exposure is a sneaky trigger.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.