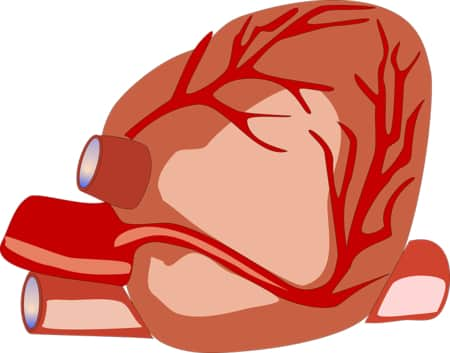
Cardiac tamponade is a clinical syndrome associated with acute impairment of cardiac function and systemic hemodynamics due to rapid accumulation of fluid in the pericardial cavity and elevation of intrapericardial pressure.
Cardiac tamponade can manifest as chest discomfort, excruciating shortness of breath, tachycardia, tachypnea, paradoxical pulse, arterial hypotension, jugular vein swelling, fainting, and shock. The diagnosis of cardiac tamponade is based on physical examination, EchoCG, ECG, chest X-ray, right heart catheterization. In case of cardiac tamponade, urgent pericardial puncture is indicated, sometimes – pericardiotomy, subtotal pericardectomy.
General information
Cardiac tamponade is a critical condition caused by increasing fluid accumulation in the pericardial cavity, a significant increase in intrapericardial pressure, violation of ventricular diastolic filling, leading to a sharp decrease in cardiac output. According to clinical manifestations, cardiac tamponade can be acute and chronic. Acute cardiac tamponade is characterized by rapid and rapid development of symptoms and unpredictable course. In cardiology, cardiac tamponade is a dangerous complication leading to severe central hemodynamic disturbances, metabolic and microcirculatory disorders, contributing to acute heart failure, shock and cardiac arrest.
Causes of cardiac tamponade
Cardiac tamponade can develop with accumulation in the pericardial cavity of different types of effusion (blood, pus, exudate, transudate, lymph), and gas. Most often acute cardiac tamponade occurs during hemopericardium – bleeding into the pericardial cavity, which develops during open and closed injuries of the chest and heart; due to medical procedures (myocardial biopsy, cardiac probing, central venous catheter placement) and surgery; during aortic aneurysm dissection, spontaneous heart rupture in patients with myocardial infarction, during treatment with anticoagulants.
Cardiac tamponade can complicate the course of pericarditis (tuberculosis, purulent, acute idiopathic), malignant tumors of heart and lungs, chronic renal failure, systemic lupus erythematosus, myxedema, etc.
Hemodynamics in cardiac tamponade
Hemodynamic disturbances in cardiac tamponade depend not so much on the volume, but on the rate of fluid inflow and the degree of pericardial distensibility. Normally, the pericardial cavity contains approximately 20-40 ml of fluid, and intrapericardial pressure is about 0 mmHg. Due to the adaptive capacity of the pericardium, slow accumulation of up to 1000-2000 ml of effusion usually results in a slight change in intrapericardial pressure.
If even a small amount (more than 100-200 ml) of exudate suddenly enters the pericardial cavity, there may be a sharp rise in intrapericardial pressure, leading to compression of the heart and intrapericardial areas of the upper and lower vena cava. Blood flow to the ventricles is obstructed, resulting in decreased filling during diastole, decreased stroke volume and cardiac output.
Normally at the end of diastole pressure in right atrium and ventricle is about 7 and 5 mm Hg respectively, in left atrium and ventricle – up to 14 and 12 mm Hg. Cardiac tamponade develops when the intrapericardial pressure becomes equal to the ventricular end diastolic pressure.
The characteristic increase in central venous pressure (CVP), increased heart rate and increased peripheral resistance is a compensatory mechanism aimed at maintaining adequate filling of the heart and its ejection. Cardiac tamponade with low intrapericardial pressure can occur with decreased intravascular volume (hypovolemia) in dehydrated patients in critical condition.
Symptoms of cardiac tamponade
Clinical manifestations of cardiac tamponade are caused by a sharp decrease in the pumping function of the heart and cardiac output. The complaints of patients with cardiac tamponade are usually non-specific: heaviness in the chest, increasing dyspnea, a feeling of “fear of death”, sharp weakness, profuse cold sweat. When the patient is examined, cyanosis of the skin, psychomotor agitation, tachycardia, rapid shallow breathing, a pronounced paradoxical pulse, arterial hypotension, muffled heart tones are noted. In acute cardiac tamponade, due to powerful activation of the sympathoadrenal system, BP can be maintained for several hours and improvement of venous return can be observed.
The clinical picture of severe acute cardiac tamponade, caused, for example, by myocardial or aortic rupture, can be manifested by sudden syncope and hemorrhagic collapse, requiring urgent surgical intervention, without which the patient dies.
With gradual development (chronic course) clinical symptoms of cardiac tamponade are similar to the manifestations of heart failure: patients are disturbed by dyspnea on exertion and in prone position (orthopnea), weakness, loss of appetite, jugular vein swelling, pain in the right subcostal area, hepatomegaly, ascites. Decompensation of stasis in the systemic circulation in chronic cardiac tamponade leads to development of shock.
Diagnosis of cardiac tamponade
The presence of cardiac tamponade can be suspected when a patient simultaneously develops dyspnea, tachycardia or tachypnea, increased CVD, low BP, paradoxical pulse with no signs of left ventricular insufficiency. A paradoxical pulse is not a characteristic symptom of cardiac tamponade and may also accompany COPD, acute attack of bronchial asthma, TELA, right ventricular myocardial infarction, and constrictive pericarditis. A paradoxical pulse may be absent in patients with cardiac tamponade with acute or chronic aortic insufficiency, ASD, severe hypotension, local myocardial compression (e.g., massive blood clots).
Echocardiography in cardiac tamponade has the highest diagnostic value, as it can detect even a small volume of effusion in the pericardial cavity, as well as diastolic collapse of right heart chambers and changes in blood flow rate through tricuspidal and mitral valves on inhalation. Transesophageal EchoCG is performed when there are signs of tamponade after cardiac surgery and when it is difficult to detect pericardial effusion.
ECG manifestations of cardiac tamponade are usually nonspecific (low amplitude of QRS complex, flattened or negative T waves, with a large volume of effusion – complete electrical alternation of P and T waves and QRS complex). Chest radiography in cardiac tamponade often reveals an enlarged heart shadow with impaired pulsation, no venous stasis in the lungs.
Right heart catheterization can confirm the diagnosis of cardiac tamponade and assess the severity of hemodynamic abnormalities. Pulsed Doppler imaging in cardiac tamponade shows the dependence of blood flow through the heart valves on respiratory excursions (decrease in transmitral blood flow on inspiration >25%, decrease in transcuspidal blood flow on exhalation >40%). Cardiac tamponade must be differentiated from constrictive pericarditis and severe myocardial insufficiency.
Treatment of cardiac tamponade
Due to life-threatening condition in all cases of cardiac tamponade, urgent evacuation of pericardial fluid by pericardial puncture (pericardiocentesis) or surgical intervention (in traumatic and postoperative genesis of tamponade) is indicated. Infusion therapy (intravenous administration of blood plasma, nootropic agents) is used to provide hemodynamic support in cardiac tamponade.
Pericardial puncture is performed under mandatory control of EchoCG or fluoroscopy, with continuous monitoring of BP, HR, CVD. A pronounced clinical effect of pericardiocentesis in cardiac tamponade is already evident with aspiration of 25-50 ml of fluid from the pericardial cavity. After removal of the effusion, antibiotics, hormones and sclerosing agents may be injected into the pericardial cavity according to indications. To prevent repeated accumulation of the effusion in the pericardial cavity a drainage for continuous outflow of fluid is inserted. Further treatment of the underlying disease is carried out to prevent the development of recurrent cardiac tamponade.
At high risk of recurrent cardiac tamponade, surgical treatment (fenestration, subtotal pericardectomy) is preferred, providing more complete drainage of the pericardial cavity. Emergency surgery for life indications is performed for tamponade due to cardiac or aortic rupture.
During fenestration, a hole is made in the pericardial wall to drain the cavity and the inner surface is inspected to detect traumatic hemopericardium or tumor foci. Subtotal pericardectomy is a radical method of cardiac tamponade treatment in chronic exudative pericarditis, scar changes and pericardial calcification.
Prognosis and prevention of cardiac tamponade
Untimely undiagnosed cardiac tamponade can be fatal. The situation is unpredictable in case of hemopericardium and cardiac tamponade in case of significant trauma or heart rupture, aortic aneurysm dissection. With early diagnosis and necessary treatment of cardiac tamponade the immediate prognosis is usually favorable, the long-term prognosis depends on the etiology of the disease.
Prevention of cardiac tamponade includes timely treatment of pericarditis, compliance with the technique of invasive procedures, monitoring of the clotting system during anticoagulant therapy, therapy of concomitant diseases.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.