Arthrosis and arthritis are two commonly misunderstood joint conditions, and while they sound similar, they are quite distinct in nature. Understanding the differences is crucial for proper diagnosis, treatment, and management.
Prevalence of Joint Conditions in the U.S.
| Condition | Prevalence (%) |
|---|---|
| Osteoarthritis (Arthrosis) | 23% |
| Rheumatoid Arthritis | 5% |
| Gout | 4% |
| Psoriatic Arthritis | 3% |
| Other Arthritis Types | 2% |
This chart highlights the prevalence of different joint conditions in the U.S., emphasizing the widespread impact of osteoarthritis compared to other forms of arthritis.
Understanding Arthrosis: A Degenerative Joint Condition
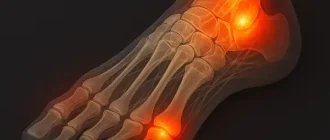
Arthrosis, also known as osteoarthritis, is a chronic condition characterized by the breakdown of cartilage in the joints. It is primarily a wear-and-tear condition associated with aging.
- Causes:
- Aging is the leading cause, as the cartilage naturally wears down over time.
- Overuse of joints due to repetitive movements or physical labor, which can accelerate joint degradation.
- Obesity, which increases stress on weight-bearing joints like knees and hips, contributing to faster cartilage breakdown.
- Past injuries or trauma to the joints, such as fractures or ligament tears, which can lead to uneven joint surfaces and faster deterioration.
- Genetic predisposition in some individuals, making them more susceptible to early cartilage loss.
- Symptoms:
- Joint stiffness, especially in the morning or after periods of inactivity, which can last longer as the condition progresses.
- Pain during or after movement, particularly after intense physical activity or prolonged use of the affected joint.
- Decreased range of motion, making everyday tasks such as climbing stairs or gripping objects more challenging.
- Joint swelling in some cases, often accompanied by tenderness and mild warmth around the joint.
- Audible creaking or cracking sounds (crepitus) during movement, caused by rough joint surfaces rubbing together.
- Commonly Affected Areas:
- Knees, which bear significant weight and are prone to overuse.
- Hips, often affected due to both weight-bearing and rotational stress.
- Hands, particularly the finger joints and the base of the thumb, where repetitive tasks take a toll.
- Spine, particularly the cervical and lumbar regions, leading to stiffness and discomfort in the neck and lower back.
Arthritis: Inflammation at Its Core
Arthritis is a broad term used to describe inflammation of the joints. It can have several types, the most common being rheumatoid arthritis (an autoimmune condition) and gout (caused by uric acid buildup).
- Causes:
- Autoimmune disorders, such as in rheumatoid arthritis, where the body’s immune system mistakenly attacks its own tissues, leading to chronic inflammation and joint damage.
- Metabolic abnormalities, like in gout, caused by an excess of uric acid in the bloodstream, which forms painful crystals in the joints.
- Infections that spread to the joints, often originating from bacterial or viral sources, can lead to septic arthritis, a medical emergency requiring immediate attention.
- Genetic predisposition in some cases, where inherited traits increase the likelihood of developing specific forms of arthritis, such as ankylosing spondylitis.
- Environmental factors, including exposure to toxins or smoking, can exacerbate autoimmune responses in individuals predisposed to conditions like rheumatoid arthritis.
- Symptoms:
- Swelling, redness, and warmth in the affected joints, often accompanied by tenderness and a sensation of heat in the area.
- Persistent joint pain, even at rest, which can interfere with sleep and daily activities, particularly in advanced stages.
- Fatigue and fever in systemic forms like rheumatoid arthritis, reflecting the condition’s impact beyond the joints and on overall health.
- Morning stiffness lasting more than 30 minutes, often described as a “gel phenomenon,” where joints feel stiff and immobile after inactivity.
- Joint deformities in chronic or untreated cases, leading to visible changes in joint shape and reduced functionality.
- Commonly Affected Areas:
- Fingers, wrists, elbows, and knees, often presenting with symmetrical involvement in conditions like rheumatoid arthritis.
- Systemic arthritis may affect multiple organs, including the lungs, heart, and eyes, requiring interdisciplinary medical management.
- Shoulders and ankles can also be impacted in specific types of arthritis, such as psoriatic arthritis or ankylosing spondylitis, which may extend to the spine.
Key Differences Between Arthrosis and Arthritis
| Feature | Arthrosis | Arthritis |
|---|---|---|
| Nature | Degenerative (wear-and-tear) | Inflammatory |
| Cause | Aging, overuse, obesity | Autoimmune, metabolic, or infectious |
| Symptoms | Stiffness, pain with movement | Swelling, redness, pain at rest |
| Progression | Gradual | Can be sudden or chronic |
| Treatment Focus | Cartilage preservation, pain relief | Reducing inflammation, immune modulation |
Symptom Onset Timeline for Arthrosis and Arthritis
This chart visualizes the progression of symptoms in arthrosis and arthritis over time, highlighting how early intervention can help manage severity.
Diagnostic Approaches
Medical professionals use distinct diagnostic methods to differentiate these conditions:
- Imaging Studies:
- Arthrosis: X-rays show joint space narrowing and bone spurs.
- Arthritis: MRI or ultrasound may reveal joint inflammation or erosion.
- Blood Tests:
- Arthrosis: No specific markers in the blood.
- Arthritis: Elevated inflammatory markers like ESR and CRP; rheumatoid factor may be positive.
- Joint Fluid Analysis:
- Can help distinguish gout from other forms of arthritis.
Treatment Strategies
Arthrosis
- Lifestyle Modifications:
- Weight management to reduce joint stress.
- Low-impact exercises like swimming and cycling to maintain joint mobility.
- Medications:
- Pain relievers like acetaminophen or NSAIDs.
- Injections of corticosteroids or hyaluronic acid for severe cases.
- Advanced Options:
- Physical therapy.
- Joint replacement surgery if the damage is extensive.
Arthritis
- Lifestyle Adjustments:
- Anti-inflammatory diets rich in omega-3 fatty acids.
- Regular but gentle exercises to reduce stiffness.
- Medications:
- Disease-modifying antirheumatic drugs (DMARDs) for autoimmune forms.
- Colchicine or urate-lowering drugs for gout.
- Advanced Options:
- Biologic therapies targeting immune system pathways.
- Joint surgeries in cases of severe damage.
Did You Know?
Arthritis affects 23% of adults in the U.S., according to the CDC, with over 58.5 million people reporting symptoms. Rheumatoid arthritis is more common in women, while gout predominantly affects men. (Source)
Exercise Impact on Joint Health
| Exercise Type | Pain Reduction (%) |
|---|---|
| Swimming | 70% |
| Cycling | 60% |
| Walking | 40% |
| Running | 30% |
This chart compares the effectiveness of different exercise types in reducing joint pain, emphasizing the benefits of low-impact activities like swimming and cycling.
Editorial Advice
For those experiencing joint pain, identifying whether the cause is arthrosis or arthritis is critical. Consult with a healthcare provider to determine the best course of action. While lifestyle changes and medications can significantly improve quality of life, early intervention remains key to managing these conditions effectively.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.