Let’s be real: hickies are one of those awkward little skin souvenirs nobody really asks for, yet they somehow manage to show up at the worst possible time. Maybe it’s the morning before a big work meeting, dinner with your parents, or even just a day when you’d prefer not to answer awkward questions. Hickies, or “love bites,” may be small, but they often feel like they come with a giant spotlight. The good news? Understanding what they are and how to deal with them can take away both the stress and the stigma.
What Exactly Is a Hickey and Why Does It Happen?
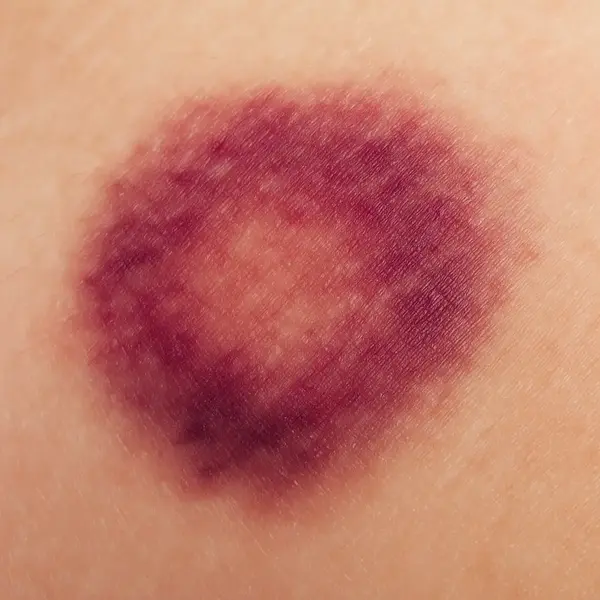
A hickey is essentially a bruise caused by suction on the skin. When someone sucks or applies pressure to an area (most commonly the neck or shoulder), tiny blood vessels just beneath the skin—capillaries—break. Blood leaks out and collects under the skin’s surface. That trapped blood appears as a reddish or purplish mark.
The healing process is similar to any bruise:
- At first, it looks dark red or purple because the blood is fresh.
- Over days, the color shifts to green, then yellow, as the body breaks down and reabsorbs the blood.
- Eventually, the mark fades completely.
In short: it’s simply broken capillaries healing over time. ⧉
Are Hickies Harmful or Just Embarrassing?
For most people, hickies are harmless and temporary. They usually fade in about 3–12 days without leaving scars. The main issue is social or cosmetic. That said, there are exceptions:
- Medical risks: In very rare cases, a strong hickey can damage a blood vessel more seriously. A published case in New Mexico described a teenager who suffered a small stroke after a hickey caused a blood clot in his neck. While this is extremely uncommon, it highlights the fact that hickies are still minor injuries.
- Skin conditions: People with clotting disorders, very fragile skin, or those taking blood thinners may notice larger or slower-healing bruises.
So, for the average healthy person, hickies are just awkward. But if something feels off, it’s worth paying attention.
Classic Home Remedies: What Works and What Doesn’t
The internet is full of hacks for hickies. Some are useful; others are little more than myths. Let’s sort through them:
What really helps:
- Cold compress (first 24 hours): Applying a cold spoon, ice pack, or even a bag of frozen peas constricts blood vessels and reduces bleeding under the skin. Hold it on the hickey for 10–15 minutes at a time.
- Warm compress (after 48 hours): Once the bruise has formed, gentle heat (like a warm towel or heating pad) helps dilate blood vessels and improve circulation, speeding recovery.
- Arnica cream or vitamin K cream: Both have evidence for helping bruises heal faster by supporting blood reabsorption.
What doesn’t really work (and why):
- Toothpaste: Some say the tingling sensation “stimulates circulation,” but dermatologists note it mostly just irritates the skin.
- Coin trick: This involves rubbing the hickey with the edge of a coin to “disperse blood.” While it may make the skin redder temporarily, it doesn’t make the bruise heal faster—and may even damage delicate skin.
- Toothbrush method: Brushing the hickey in circles with a stiff toothbrush is another popular myth. In reality, it can break even more capillaries and worsen the bruise.
As Reyus Mammadli, medical consultant, explains: “It’s important to understand why a method works or doesn’t. Cold compresses help because they limit bleeding. Warm compresses help because they improve circulation later. Coins and toothpaste don’t work because they don’t change the healing process—they only irritate the skin.” ⧉
Medical Treatments for Faster Recovery
Sometimes you don’t have a week to wait for a bruise to fade. Dermatology offers options that actually work and deliver results faster. Here’s a detailed look:
Laser Therapy
Laser therapy is one of the most effective ways to remove a hickey quickly. A dermatologist uses a specialized vascular laser that targets hemoglobin (the pigment in blood). The laser breaks down the blood under the skin, allowing the body to absorb it more efficiently.
- How it works: Short bursts of light are directed at the bruise, breaking down blood pigments.
- Duration: Each session takes about 10–15 minutes.
- Pain level: Patients often describe it as a mild snapping sensation, similar to a rubber band on the skin.
- Sessions needed: Usually 1–2 sessions are enough.
- Effectiveness: 9/10, with visible fading within 24–48 hours.
- Average cost in the U.S.: $150–$300 per session.
Topical Retinoids
Retinoids, such as tretinoin cream, are prescription-strength medications that speed up cell turnover. By encouraging skin renewal, they can help a hickey fade more quickly.
- How it works: Applied directly to the hickey once daily.
- Duration: Takes several days of application to see results.
- Pain level: Usually painless but may cause mild dryness or peeling.
- Effectiveness: 6/10, best for people who want to boost natural healing.
- Average cost in the U.S.: $50–$150 for a prescription tube.
Hydroquinone Creams
Hydroquinone is often prescribed to lighten areas of hyperpigmentation. While not specifically designed for bruises, it can help reduce lingering discoloration after a hickey.
- How it works: Blocks the production of melanin, lightening the skin over time.
- Duration: Results are gradual, often taking 1–2 weeks.
- Pain level: Usually none, but some people experience mild skin irritation.
- Effectiveness: 5/10, more useful if discoloration remains after the bruise fades.
- Average cost in the U.S.: $30–$100 depending on concentration and brand. ⧉
How Long Do Hickies Last Without Treatment?
The healing timeline depends on age, circulation, and skin tone, but usually falls between 3–12 days.
Typical stages:
| Stage | Color | Timeline (Days) |
|---|---|---|
| Fresh | Red/Purple | 1–2 |
| Mid | Green | 3–5 |
| Late | Yellow/Brown | 6–9 |
| Fading | Light Yellow | 10–12 |
Why does the color change? It’s your body breaking down hemoglobin (blood pigment) into different components—biliverdin (green) and bilirubin (yellow)—until the bruise disappears.
When Should You Actually See a Doctor?
Most hickies don’t need medical attention. But there are situations where it’s safer to see a doctor. Each red flag comes with its own reasoning and steps for action:
- The bruise is unusually large, painful, or swollen. Mild tenderness is normal for any bruise, but if the pain feels sharp, constant, or the area swells more than expected, it may point to deeper tissue injury or a clot. If after 2–3 days the pain is not easing, that’s a good moment to schedule an exam.
- It doesn’t improve after 2 weeks. A typical hickey fades in 3–12 days. If the mark is still dark and prominent after two weeks, it may not be a hickey at all, but another type of lesion or vascular issue. A dermatologist can rule out more serious conditions.
- You notice numbness, weakness, or dizziness nearby. Numbness or tingling around the bruise, or weakness in the arm or face on the same side, can suggest that blood flow has been compromised. These symptoms are urgent—seek emergency care right away.
- You’re on blood thinners or have a clotting disorder. In this case, even a small bruise can expand quickly and cause complications. If you see that the hickey keeps spreading in size, or new bruises appear without clear cause, call your physician promptly. Monitoring your medication’s effect on bruising is an important part of managing your health.
As Reyus Mammadli advises: “If a hickey feels different from a typical bruise—harder, more painful, or spreading—it’s better to get checked than to ignore it.”
Can You Prevent Hickies in the First Place?
Yes, and prevention is often about being proactive:
- Gentleness: Less suction and pressure means fewer broken capillaries.
- Choose the spot wisely: The neck and collarbone bruise easily. Areas with thicker skin are less likely to show marks.
- Communication between husband and wife: Talk openly with your spouse. Prevention often starts with setting boundaries and being clear about comfort levels.
- Clothing tricks: Scarves and turtlenecks won’t prevent hickies but can help cover them if prevention fails.
Editorial Advice
Reyus Mammadli, medical consultant, emphasizes a simple, science-backed approach: “Start cold, then go warm. Support healing with topical creams. And if you need rapid results, lasers work.”
Our editorial team also recommends:
- Stay hydrated and eat foods rich in vitamin C and K, which support blood vessel health.
- Avoid skin trauma from harsh scrubbing or rubbing.
- If hickies are a recurring concern, think prevention—not just treatment.
At the end of the day, hickies are temporary. They fade, they heal, and they’re usually more embarrassing than dangerous. A mix of patience, good skincare, and maybe a little humor is often the best remedy.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.