Colitis is a term used to describe inflammation of the colon, or large intestine. This condition can cause a variety of uncomfortable symptoms, including abdominal pain, diarrhea, and fatigue. Colitis can result from infections, autoimmune diseases, or other underlying health issues. Understanding colitis is essential, as it can lead to complications like dehydration or colon damage if left untreated.
Frequency of Different Types of Colitis
| Type | Frequency (%) |
|---|---|
| Ulcerative Colitis | 45% |
| Crohn’s Disease | 35% |
| Infectious Colitis | 15% |
| Ischemic Colitis | 5% |
This chart illustrates the relative frequency of various types of colitis, highlighting the prevalence of ulcerative colitis and Crohn’s disease compared to less common forms like ischemic colitis.
Early Signs of Colitis That Could Save Your Health
Recognizing the early signs of colitis can make a significant difference in managing the condition effectively. Common symptoms include:
- Persistent diarrhea, often accompanied by blood or mucus, can disrupt daily life and may lead to dehydration if untreated. Imagine needing to use the bathroom multiple times an hour—this level of urgency is a common complaint among colitis sufferers. Additionally, spotting blood or mucus in stool can be alarming and is a clear sign to consult a doctor.
- Abdominal cramps and bloating often feel like a constant ache or sharp pains that come and go. These symptoms can make it hard to eat, as even small meals may trigger discomfort. Patients often describe it as a feeling of being “full” or “gassy” all the time, despite having an empty stomach.
- Fatigue or unexplained weight loss is more than just feeling tired; it’s the kind of exhaustion that makes everyday tasks feel impossible. For example, a 28-year-old from Austin reported struggling to work due to constant fatigue and losing 15 pounds in just two months without changing her diet.
- Fever, particularly in severe cases, is the body’s way of signaling inflammation. Unlike a mild flu-like fever, colitis-related fevers are often accompanied by chills and a sense of malaise. One patient from Seattle noted that her fevers felt like they “drained all energy,” leaving her bed-bound for days.
If these symptoms persist, seeking medical advice is crucial. Prompt diagnosis and treatment can prevent the condition from worsening.
Comparison of Flares and Remissions in Colitis Cases
| Phase | Frequency (%) |
|---|---|
| Flares | 60% |
| Remissions | 40% |
This chart compares the frequency of flares (60%) versus remissions (40%) in patients with colitis, illustrating the challenges of achieving long-term symptom control.
Debunking Colitis Myths: It’s Not Just About Food
A common misconception is that colitis is solely caused by diet. While certain foods can exacerbate symptoms, colitis often stems from deeper issues such as:
- Autoimmune responses, as seen in ulcerative colitis and Crohn’s disease.
- Bacterial or viral infections.
- Ischemic colitis, caused by reduced blood flow to the colon.
Understanding the root causes of colitis is key to proper management and avoiding unnecessary dietary restrictions.
The Different Types of Colitis and How They Impact You
| Type of Colitis | Causes | Symptoms | Treatment Options |
|---|---|---|---|
| Ulcerative Colitis | Autoimmune reaction targeting colon lining | Chronic diarrhea, rectal bleeding, pain | Anti-inflammatory drugs, biologics, surgery |
| Crohn’s Disease | Autoimmune reaction affecting any GI part | Abdominal pain, weight loss, fistulas | Immunosuppressants, biologics, surgery |
| Infectious Colitis | Bacterial, viral, or parasitic infections | Diarrhea, fever, abdominal cramps | Antibiotics, hydration |
| Ischemic Colitis | Reduced blood flow to the colon | Sudden pain, visible blood in stool | Supportive care, surgery in severe cases |
| Microscopic Colitis | Unknown, often linked to autoimmune factors | Chronic watery diarrhea | Anti-inflammatory drugs, lifestyle changes |
This table offers a detailed comparison of the types of colitis, helping patients and readers identify potential symptoms and seek appropriate treatments.
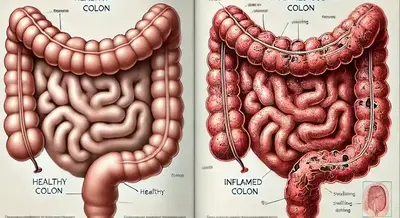
What Happens Inside Your Body When You Have Colitis
When colitis occurs, the body’s immune system or external pathogens attack the colon’s lining. This leads to:
- Inflammation and swelling of the tissue are the body’s immediate responses to the perceived threat in the colon, often caused by infections, autoimmune reactions, or injuries. For instance, in ulcerative colitis, the immune system mistakenly targets the colon’s lining, causing persistent inflammation.
- Damage to the protective mucus layer exposes the delicate inner lining of the colon to harmful bacteria and toxins. This can lead to ulcer formation. A vivid example is seen in severe infectious colitis caused by Clostridioides difficile, where toxins disrupt the mucus barrier, resulting in pain and persistent diarrhea.
- Symptoms like pain, diarrhea, and bleeding occur as the colon struggles to heal and defend itself. For example, patients with ischemic colitis often experience sudden abdominal pain and visible blood in stools due to reduced blood flow compromising the healing process. These symptoms are the body’s way of signaling distress and inflammation.
In severe cases, this process can cause ulcers or perforations in the colon, requiring immediate medical intervention.
Effective Treatment Options for Colitis: From Medications to Surgery
Treatment depends on the type and severity of colitis but often includes:
- Medications:
- Anti-inflammatory drugs: Medications such as mesalamine and sulfasalazine are commonly prescribed to reduce inflammation in the colon.
- Immunosuppressants: Drugs like azathioprine or methotrexate help control the immune system’s overreaction.
- Biologic therapies: Medications such as infliximab or adalimumab target specific proteins involved in inflammation, offering relief for severe cases.
- Antibiotics: Used for infectious colitis, these help eliminate harmful pathogens in the colon.
- Dietary Adjustments:
- While not curative, adjusting diet to avoid trigger foods (e.g., spicy or high-fiber foods during flare-ups) can alleviate symptoms.
- Surgery:
- For severe cases where medication fails, surgical options include colectomy (removal of part or all of the colon).
- Procedures may involve minimally invasive laparoscopic techniques, reducing recovery time.
Effectiveness of Colitis Treatment Methods
This horizontal bar chart highlights the effectiveness of various colitis treatment methods, with surgery showing the highest success rate at 90%, while antibiotics for infectious colitis are less effective overall at 40%.
Effectiveness and Costs:
- Medications: Biologic therapies have an effectiveness rate of 60–70% in reducing symptoms, with costs ranging from $2,000 to $6,000 per dose.
- Surgery: Colectomy success rates are high, exceeding 90% in restoring quality of life. Costs vary but typically range from $20,000 to $50,000.
Modern therapies, like biologic drugs, offer hope for patients by targeting specific immune pathways.
Recovery Speed After Different Treatments
| Treatment Type | Recovery Speed (Weeks) |
|---|---|
| Biologic Therapies | 8 Weeks |
| Anti-inflammatory Drugs | 6 Weeks |
| Immunosuppressants | 4 Weeks |
| Surgery (Colectomy) | 9 Weeks |
This chart illustrates the average recovery speed after various treatments for colitis, highlighting differences in duration and effectiveness.
Living Well with Colitis: Practical Tips and Real Stories
Living with colitis requires adjustments, but many lead fulfilling lives. Practical tips include:
- Keeping a symptom diary to identify triggers, such as specific foods, stress, or medications, can help patients anticipate and avoid flare-ups. For example, a 45-year-old man from Chicago found that tracking his symptoms revealed stress at work as a significant trigger for his ulcerative colitis.
- Staying hydrated and prioritizing rest during flare-ups is crucial. Replenishing fluids lost during diarrhea can prevent dehydration, while adequate rest supports the body’s recovery. A woman in her 50s from Atlanta shared how incorporating short midday breaks improved her energy during active symptoms.
- Joining support groups for emotional and practical support can provide valuable insights and reduce feelings of isolation. Many patients report benefiting from shared experiences and tips. For instance, a young man in New York City mentioned that connecting with peers managing Crohn’s disease helped him navigate his treatment options more effectively.
Real stories highlight resilience: one patient, a 32-year-old woman from Denver, managed her ulcerative colitis with biologics and lifestyle changes, maintaining her active career and family life.
Understanding Colitis Risk Factors: Are You at Risk?
Certain factors increase the risk of colitis, such as:
- Family history of inflammatory bowel disease (IBD).
- Smoking or previous gastrointestinal infections.
- Age, with some forms like ulcerative colitis often appearing in young adults.
Reducing these risks involves maintaining a healthy lifestyle and monitoring gut health proactively.
Duration of Symptoms Without Treatment
| Type of Symptom | Average Duration (Weeks) |
|---|---|
| Persistent Diarrhea | 8 Weeks |
| Abdominal Pain | 6 Weeks |
| Fatigue | 5 Weeks |
| Rectal Bleeding | 7 Weeks |
This chart displays the average duration of key symptoms of colitis without treatment, emphasizing the prolonged impact on quality of life.
The Future of Colitis Treatment: Promising Research and Innovations
Research is advancing in areas like microbiome therapy and precision medicine. For example:
- Fecal microbiota transplants (FMT): Show promise in restoring gut health.
- Genetic studies: Aim to uncover specific markers for tailored treatments.
These innovations offer hope for improved outcomes and quality of life for colitis patients.
Colitis Prevention: Small Steps for a Healthier Gut
While not all cases are preventable, you can lower your risk by:
- Eating a balanced diet rich in fiber and low in processed foods.
- Staying hydrated and managing stress.
- Seeking regular medical checkups if you have a family history of IBD.
Prevention begins with awareness and proactive care.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.