Renal adenocarcinoma is a renal cell carcinoma originating from the epithelium of the tubules of the kidney. Its manifestations are lumbar pain, hematuria, increased kidney size, anemia, and cachexia.
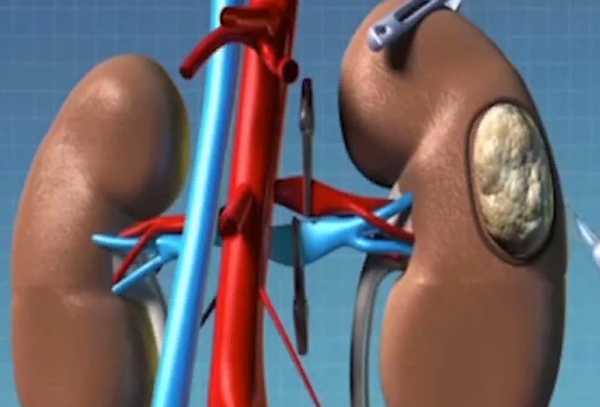
The tumor may metastasize to the lungs, paracaval and para-aortic lymph nodes, bones, liver, adrenal glands, and the opposite kidney. Pathology is diagnosed by renal ultrasound, cystoscopy, excretory urography, ureteropyelography, and renal CT. Morphological verification of the diagnosis is performed by puncture biopsy of the kidney and histological examination of the biopsy specimen. Detection of adenocarcinoma of the kidney is an indication for nephrectomy followed by radiotherapy.
General information
Renal adenocarcinoma accounts for about 2.5% of neoplasias of various localizations. In modern urology, adenocarcinoma is the most common histotype of kidney cancer in adults. Adenocarcinoma accounts for 90% of all renal tumors. The disease usually develops between the ages of 40-70 years; it affects the left and right kidney with equal frequency; it is diagnosed twice as often in men.
Causes
Renal adenocarcinoma has a polyetiological and not fully clarified nature. Renal diseases (glomerulonephritis, pyelonephritis), trauma; influence of chemical agents (nitrosoamines, hydrocarbons, aromatic amines), radiation exposure, intoxications (smoking) on renal tissue play a certain role in tumor development. Neoplasia often develops from benign adenoma of the kidney, so all detected kidney neoplasms are subject to removal and histological examination. Correlation of adenocarcinoma with obesity and hypertension has been noted. Rarely, the causes of tumor development are dysontogenetic disorders, hereditary forms of kidney cancer.
Cancer cells provoke the destruction of healthy kidney tissue, at the expense of which they later grow. Toxins released during tumor growth lead to poisoning of the body, which can be fatal. For example, approximately 40% of patients diagnosed with renal cell cancer die due to the progression of the disease, so this tumor is ranked among the deadliest malignant neoplasms.
Kidney cancer in children
Of all malignant kidney tumors in children, fetal nephroblastoma or Wilms’ tumor is the most common. It accounts for approximately 90% of all kidney tumors in children.
Characteristics of nephroblastoma:
- The tumor grows rapidly and rapidly metastasizes;
- in 2% of cases it is familial in nature;
- occurs more often in children aged 2-5 years;
- 10% of cases occur in children with malformations;
- In 6-10% of cases it affects both kidneys;
- in 2% of cases, it affects the horseshoe kidney.
Wilms’ tumor is most common in children aged 2-5 years, rare in newborns, and even rarer in children older than 8 years.
Risk factors
At this time, reliable causes of kidney cancer have not been established, but risk factors affecting the development of the cancer have been fairly accurately identified. These include:
- Smoking, both active and passive – the risk of developing the disease is increased by 50%;
- long-term intake of diuretics – by 30%;
- increased body weight (metabolic syndrome) – by 20%;
- High blood pressure – by 20%;
- Occupational exposures (work with chemicals, dyes);
- diabetes mellitus;
- long-term hemodialysis therapy;
- viral hepatitis;
- Genetic predisposition (presence of kidney cancer in first-line relatives);
- polycystic kidney disease;
- Hippel-Lindau disease.
With moderate alcohol consumption there is a protective effect (mechanism not established). Nephrosclerosis is a background disease that contributes to the development of renal cell cancer. Chronic pyelonephritis, polycystic disease, chronic kidney disease, and diabetes mellitus influence the development of nephrosclerosis.
How often does kidney cancer occur
The annual increase in kidney adenocarcinoma worldwide is due to increased life expectancy and improved diagnostic techniques (ultrasound, CT scan). Every year kidney adenocarcinoma affects more than 20 thousand Russians, 64 thousand Americans, 10 thousand people living in the UK. Even more people suffering from kidney adenocarcinoma are registered in Germany and Scandinavia.
In 2016, the incidence of kidney adenocarcinoma was noted in 4.8% of the male and 3.3% of the female population relative to the overall structure of malignant diseases. Most often at diagnosis the first and second stages of cancer are detected. Men are in the oncological risk group, because they are twice as likely to develop kidney adenocarcinoma as women. In the ranking of common diseases among men, renal cell cancer ranks eighth.
According to observations, kidney adenocarcinoma occurs more often in urban population than in rural population. In 2016, the average age of patients diagnosed with kidney adenocarcinoma for the first time in their lives was 62, and the age at which the disease reaches its peak was in the 60-70 age range.
Pathanatomy
Macroscopically, adenocarcinoma of the kidney looks like a node of soft elastic consistency. On dissection, interspersed areas of hemorrhage and necrosis are visible, giving the tumor a mottled appearance. Tumor growth may be multidirectional – in the direction of renal capsule or calyx-lobar complex; rather quickly adenocarcinoma infiltrates renal veins, inferior vena cava, adjoining tissues; it metastasizes to lymph nodes, lungs, bones, liver, brain. The microscopic structure is represented by bands and clusters of polygonal cells with a light protoplasm containing glycogen and lipids; the tumor stroma is weakly expressed.
Classification
Renal adenocarcinoma is a type of renal cell carcinoma (hypernephroid cancer) and can have different degrees of differentiation. The international TNM classification system distinguishes the following stages of the pathology:
- T1 – tumor spread is limited to the renal capsule
- T2 – tumor invasion into the fibrous capsule of the kidney
- T3 – vascular pedicle or paranephral fatty tissue is involved in tumor progression
- T4 – the tumor has invaded the nearest organs;
- Nx – preoperative evaluation of regional lymph nodes is impossible
- N1 – regional metastasis is determined by radiological or radioisotopic methods
- M0 – no distant metastases
- M1 – a single distant metastasis is detected
- M2 – multiple distant metastases are detected.
Distant metastases are detected in 50% of patients, and tumor invasion into the renal vein – in 15%. More often distant metastases are located in the lungs (54%), regional paracaval and para-aortic lymph nodes (46%), bone skeleton (32%), liver (36%), opposite kidney (20%), adrenal glands (16%). Metastases can manifest clinically even before the primary focus is detected or can occur long after nephrectomy for renal cancer. The clinical course of adenocarcinoma of the kidney is distinguished by a latent period, as well as periods of local and general manifestations.
Symptoms of adenocarcinoma of the kidney
In the latent period, clinical manifestations are absent. The development of local symptoms is accompanied by the appearance of macrohematuria and pain, enlargement of the kidney. Hematuria is noted in 70-80% of patients with adenocarcinoma of the kidney. Urinary blood secretion occurs unexpectedly, more often in the form of thread-like clots 2.5 in (6-7 cm) long. Hematuria is usually episodic, stopping and resuming. In case of intense renal bleeding (profuse hematuria), renal vein thrombosis, bladder blockage (tamponade) and acute urinary retention may occur.
Pain syndrome occurs in 60-70% of cases. The pain is dull, nagging, localized in the lower back, irradiates to the groin and thigh; at the height of hematuria it can increase to renal colic. The kidney is enlarged in 75% of cases. In the later stages, a tumor palpable through the abdominal wall is detected. When adenocarcinoma invades the venous vessels, varicose dilation of the labia and varicocele in men is observed in women.
During the period of general manifestations weight loss, weakness, hypertension progress, unexplained steady increase of body temperature, anemia, cachexia are registered. In advanced stages, paraneoplastic amyloidosis and nephrotic syndrome (generalized edema, massive proteinuria, hypoproteinemia, hypoalbuminemia, etc.) develop.
Diagnosis
Laboratory and instrumental methods are used in the diagnosis of adenocarcinoma of the kidney. General urinalysis reveals marked hematuria, moderate proteinuria; in the blood – normochromic anemia, increased sedimentation rate. The leading role in detecting adenocarcinoma of the kidney is assigned to ultrasound, endoscopic and X-ray diagnostics. Renal ultrasound is an informative method to confirm adenocarcinoma, which in addition to visualizing the tumor allows to perform puncture biopsy of the kidney with the intake of tumor tissue for morphological study of the biopsy specimen.
Cystoscopy is used at the time of hematuria, which allows to identify the ureter, from which blood is excreted. Performance of excretory urography allows to consider uneven contours and increased size of the kidney, to reveal deformation, amputation of calyces, deviation of ureters, defects of pelvis filling. In some cases retrograde ureteropyelography, renal angiography, nephroscintigraphy are indicated.
CT scan of abdominal and retroperitoneal organs. Adenocarcinoma of the left kidney with typical accumulation and washout of contrast
The fact of distant metastasis of adenocarcinoma is established by lung radiography, skeletal scintigraphy, ultrasound of the liver, adrenal glands and retroperitoneal space. The neoplasm is differentiated from renal calculi disease, renal adenoma, chronic glomerulonephritis, pionephrosis, renal tuberculosis, polycystic disease.
Because of the nonspecificity of the symptoms of renal adenocarcinoma, and sometimes their complete absence, the diagnosis is almost always established on the basis of laboratory and instrumental examination data. Foreign cancer centers detect renal adenocarcinoma with 100% accuracy and in three out of four cases – at early stages. For this purpose, the following tests are performed:
- General and biochemical blood tests, during which anemia, elevated levels of creatinine, alkaline phosphatase, and calcium may be detected;
- ultrasound examination of retroperitoneal organs, which allows determining changes in the size and shape of the kidney, localization, size, structure, and other physical characteristics of all neoplasms in it, including information on their density and consistency. The method is often used as a navigational aid when performing a percutaneous kidney biopsy;
- Excretory urography is an X-ray examination of the urinary system with intravenous injection of a contrast agent. It is used to visualize tumors, clarify the causes of hematuria (blood discharge with urine), and determine the localization and causes of urine outflow blocks;
- Multispiral computed tomography, magnetic resonance imaging with and without contrast enhancement, positron emission computed tomography – all these computerized methods of high-precision imaging both with and without the use of X-rays provide maximum information about the tumor in the kidney, its immediate and distant metastases. They are also used to plan upcoming surgery, detect early stages of recurrence or metastases after treatment, and monitor needle position in percutaneous biopsies;
- Biopsy followed by histological, histochemical, cytogenetic studies are always performed during surgical removal of the tumor. But sometimes if such surgery is not possible, or it is necessary to clarify the tissue characteristics of the tumor before surgery, a percutaneous biopsy or diagnostic laparoscopy with a sample of the tumor is performed.
Treatment of adenocarcinoma of the kidney in specialized foreign clinics is performed in strict compliance with international standards, developed for each stage of the disease and taking into account individual characteristics of the patient.
Treatment of adenocarcinoma of the kidney
With this pathology is optimal combined treatment, including radical surgery on the kidney and radiation therapy. In the early stages, a partial nephrectomy can be performed. If the process is widespread, a total nephrectomy is performed, removing the paranephral and retroperitoneal tissue with regional lymph nodes. Tumor invasion of inferior vena cava and even the presence of single distant metastases do not prevent nephrectomy. If there are single metastases in the lungs, the second stage is removal of the metastatic nidus. A combination of surgery and radiation treatment increases survival in adenocarcinoma of the kidney.
Total cancerous lesions of both kidneys may require binephrectomy with transfer to hemodialysis. The disseminated form of adenocarcinoma of the kidney, characterized by extensive metastasis and tumor overgrowth, involves symptomatic and palliative treatment with radiation and chemotherapy.
Surgery
Surgical treatment is the leading method at any stage of tumor development, and in the initial stages it is often the only necessary treatment. Surgeries are performed:
- Classical access to the retroperitoneal space;
- Laparoscopic method through a few short incisions-incisions – for small, clearly localized tumors without local spreading. This method is most often used in foreign clinics;
- using the Da Vinci robotic surgery system.
If the tumor size does not exceed 4 cm, it is localized in one of the kidney poles and does not spread further, the tumor is resected with preservation of the adrenal gland and most of the kidney.
More common variants of adenocarcinoma require complete removal of the kidney (nephrectomy) with the adrenal gland, regional lymph nodes, peri-renal tissue and tumor vein clots.
The artery feeding the affected kidney is often embolized before such surgery. This helps to stop the blood supply to the tumor, reduce the size of the organ, and reduce blood loss during the operation. Embolization is performed percutaneously, using a catheter inserted through the peripheral artery under fluoroscopy. Such interventions are performed by endovascular surgeons in radiology operating theatres, which are available at all modern foreign cancer centers.
If radical surgery is contraindicated for the patient, percutaneous radiofrequency ablation of the tumor is performed. A radio-wave source in the form of a thin probe is introduced into the adenocarcinoma under the control of imaging techniques. When a high-frequency current is applied to it, it heats up and coagulates the tumor tissue.
After surgery
After laparoscopic surgery, recovery is much faster and the patient feels almost no pain. There are small incisions in the skin, which heal quickly. You will be able to get up and eat after the first day, which will speed up your recovery. And you will be discharged from the hospital on day 2-3. Rehabilitation takes 1-2 months.
After open surgery, it will not be easy because of the cut muscles or even removed ribs. On average, it takes anywhere from 1 week to 1 month before you are allowed to go home. But rehabilitation will last about 1.5 years. You will be prescribed pain medication, recommended moderate physical activity to restore blood circulation, and prescribed a special diet. After surgery, you will need to visit your urologist regularly for follow-up examinations and undergo a CT scan once every six months.
How long you live after surgery for kidney cancer depends on the type and stage of the cancer, as well as how the surgery is performed.
Prognosis
After nephrectomy, patients are monitored by a urologist and undergo dynamic lung X-rays for early detection of metastases. Long-term prognosis is unfavorable: there is a high percentage of late tumor metastasis to bones and lungs. After total nephrectomy the 5-year survival rate is overcome by 40-70% of patients. To exclude the probability of adenocarcinoma of the kidney, it is recommended to maintain a healthy lifestyle, avoid bad habits, timely treatment of kidney disease. Prophylactic ultrasound examination of the kidneys and immediate visit to a nephrologist (urologist) in case of pain in the lower back or blood in the urine are necessary.
There is no exact prognosis for survival, it depends greatly on the accompanying factors: other diseases, the environment, the size and shape of the tumor, the psychological state of the patient. The most important thing is timely qualified medical care, which you can receive at our medical center.
What are the numbers?
90% of kidney cancer detected in the first stage can be cured. The survival rate of a patient with stage 4 cancer with metastases is usually less than 1 year.
The chance of living 5 years after diagnosis in the first and second stages is 76% and 54%, respectively, in the third stage is already 42%, in the fourth – about 10%.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.