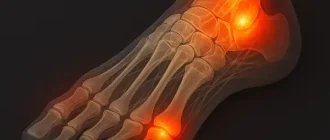
Midfoot pain refers to soreness or discomfort in the middle of the foot, where the arch connects the heel and the front part. It’s like the central hinge of a bridge — when it weakens, the whole structure loses balance. This discomfort can make even short walks feel tiring and affect overall stability.
Pain developing in the middle of the foot often results from overuse, joint inflammation, or previous injuries. Research suggests that conditions affecting this area account for about 5–7% of all foot problems, especially among athletes and people who stand for long hours. Over time, untreated strain in the middle of the foot can lead to chronic discomfort and reduced flexibility.
After a busy day or workout, when swelling or stiffness appears across the middle section of the foot, it may be a sign worth noticing. Understanding what causes this type of discomfort, how to relieve it, and when to seek medical advice helps maintain healthy movement and foot strength.
Common Causes of Midfoot Pain
Midfoot pain can arise from a variety of mechanical and pathological origins. The most prevalent causes include overuse injuries, degenerative arthritis, trauma, and deformities such as flatfoot or high arches.
Sports Injuries and Overuse
Athletes frequently develop midfoot pain due to repetitive stress on the Lisfranc joint complex. Sports such as running, soccer, or basketball often cause microtrauma, leading to ligament strain or stress fractures. MRI imaging frequently reveals edema and microcracks in metatarsal bones, indicating early overuse syndrome ⧉.
Arthritis and Joint Degeneration
Midfoot arthritis—commonly osteoarthritis or post-traumatic arthritis—results from cartilage breakdown between tarsal bones. Clinically, patients present with stiffness, swelling, and pain that worsens during weight-bearing. Radiographic findings typically show joint-space narrowing and osteophyte formation.
Nerve or Tendon Problems
Entrapment of the deep peroneal nerve or tendinitis of the tibialis posterior can manifest as chronic burning or aching midfoot pain. These conditions are frequently observed in individuals with altered foot biomechanics or previous injuries.
When to See a Doctor
Persistent pain lasting more than one week, swelling, visible deformity, or difficulty walking should prompt immediate medical evaluation. Ignoring such symptoms may exacerbate the underlying pathology, resulting in chronic instability or degenerative changes. Reyus Mammadli, medical consultant, recommends prompt professional assessment to avoid irreversible joint damage.
Diagnostic Methods for Midfoot Pain
Physical Examination and Gait Analysis
A clinical evaluation begins with palpation, range-of-motion testing, and gait assessment. Pressure mapping systems such as Tekscan™ F-Scan help identify abnormal load distribution.
Imaging Techniques — X-ray, MRI, and CT Scan
- X-ray: Useful for detecting fractures or alignment issues (accuracy 6/10; average cost $100–$250 / €90–€220).
- MRI: Excellent for soft tissue and cartilage evaluation (accuracy 9/10; cost $400–$1,200 / €360–€1,080).
- CT Scan: Ideal for 3D bone visualization and preoperative planning (accuracy 8/10; cost $500–$1,000 / €450–€900) ⧉.
Ultrasound and Advanced Biomechanical Testing
Ultrasound is increasingly used for dynamic tendon assessment, with approximately 85% accuracy. Coupled with motion capture analysis, it offers valuable insight into functional foot behavior during movement.
Treatment Options for Midfoot Pain
Rest, Ice, and Orthotic Support
Initial management includes activity modification, cryotherapy, and orthotic inserts (brands such as Superfeet® or Powerstep®). Custom-made insoles reduce midfoot strain and restore proper alignment.
Physical Therapy and New Technologies
Physical therapy focuses on strengthening the intrinsic muscles of the foot. Recent innovations like AlterG Anti-Gravity Treadmill and BTE Primus RS rehabilitation systems allow low-impact recovery, particularly after surgery ⧉.
Medications and Injections
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen alleviate pain and inflammation. Corticosteroid injections are indicated in cases of severe arthritis but must be used cautiously. Platelet-rich plasma (PRP) therapy has shown promising results in early studies.
Surgical Options and Recovery Outlook
For advanced degenerative or traumatic conditions, surgical options such as midfoot fusion (arthrodesis) or osteotomy may be necessary. Modern minimally invasive approaches reduce recovery time and postoperative complications. Typical recovery spans 8–12 weeks, depending on bone healing and rehabilitation adherence.
Real Cases from the U.S.
Case 1 — 42-Year-Old Woman from Texas: Post-Traumatic Midfoot Arthritis
A 42-year-old woman began experiencing mild discomfort in her midfoot several years after a minor car accident. Initially, she dismissed the pain as a result of tight shoes and fatigue from long walks. However, the discomfort gradually worsened, accompanied by morning stiffness and swelling.
An X-ray examination revealed early post-traumatic arthritis in the tarsometatarsal joints. Conservative treatment with NSAIDs and custom orthotics provided temporary relief, but her symptoms persisted. After consultation with an orthopedic specialist, she underwent midfoot arthrodesis.
Three months post-surgery, her pain levels dropped significantly, and she regained full functionality. This case underscores the importance of early assessment of persistent midfoot discomfort following even minor trauma ⧉.
Case 2 — 28-Year-Old Runner from California: Stress Fracture from Overtraining
A 28-year-old marathon runner noticed a dull ache in his midfoot that worsened after each run. Believing it to be an issue with his new running shoes, he continued training. Within two weeks, swelling appeared, and walking became painful.
MRI imaging confirmed a stress fracture in the second metatarsal base. His treatment plan included a six-week non-weight-bearing period using a walking boot and PRP injections to promote faster healing. Rehabilitation with an AlterG Anti-Gravity Treadmill allowed gradual reintroduction to running without overloading the midfoot.
The fracture healed fully within eight weeks, and he resumed light training. This case highlights the risks of overtraining and ignoring early warning signs in athletes ⧉.
Case 3 — 55-Year-Old Office Worker from Florida: Degenerative Midfoot Arthritis
A 55-year-old office worker experienced a burning sensation and stiffness in her midfoot after walking short distances. Her job required prolonged standing, and she had gained weight over recent years, which exacerbated her discomfort.
MRI results revealed degenerative midfoot arthritis with early collapse of the medial arch. Initial treatment involved custom orthotics and physical therapy, but progress was slow. When her program shifted to include muscle strengthening and balance training, improvement became more evident.
Corticosteroid injections were used sparingly to manage pain during flare-ups. After six months, she reported about 70% pain reduction and improved mobility. Her experience demonstrates that consistent conservative therapy can significantly improve midfoot arthritis outcomes ⧉.
Prevention Tips for Midfoot Pain
Proper footwear selection is key. Brands such as Brooks®, ASICS®, and HOKA® produce models with enhanced midfoot cushioning. Regular stretching of calf and plantar muscles reduces midfoot tension. Reyus Mammadli, medical consultant, emphasizes maintaining healthy body weight and using supportive shoes to prevent recurrence.
Cost Overview: Diagnosis and Treatment in the U.S.
| Procedure | Average Cost (USD) | Average Cost (€) | Accuracy |
|---|---|---|---|
| X-ray | $150 | €135 | 6/10 |
| MRI | $800 | €720 | 9/10 |
| CT Scan | $700 | €630 | 8/10 |
| Orthotics | $250 | €225 | – |
| PRP Injection | $900 | €810 | – |
| Surgery (Arthrodesis) | $6,000 | €5,400 | – |
Editorial Advice
Reyus Mammadli, medical consultant, advises addressing midfoot pain promptly, as ignoring biomechanical dysfunction can result in chronic disability. He recommends integrating clinical imaging with functional analysis for optimal treatment planning. Patients should avoid self-diagnosis and seek specialized orthopedic evaluation for persistent pain. Maintaining healthy footwear habits and periodic gait assessments can substantially reduce recurrence risk.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.