Many women are familiar with pain in one of the ovaries: right or left. In this article, we will analyze the causes, methods of diagnosis and treatment of pain in the left ovary (in most cases, this also applies to pain in the right ovary.)
What Is Ovary Pain?
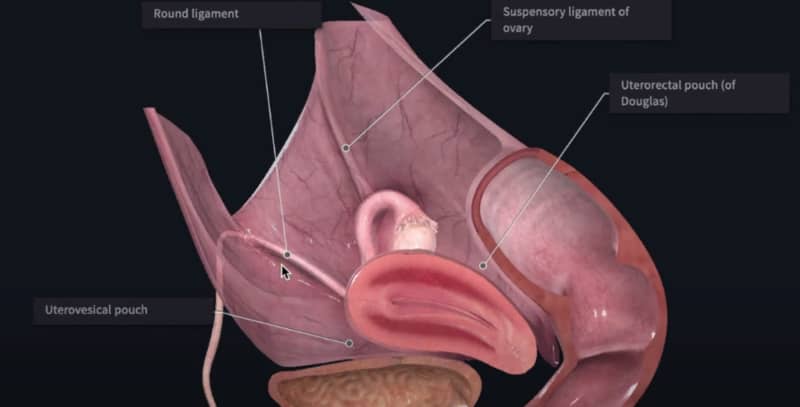
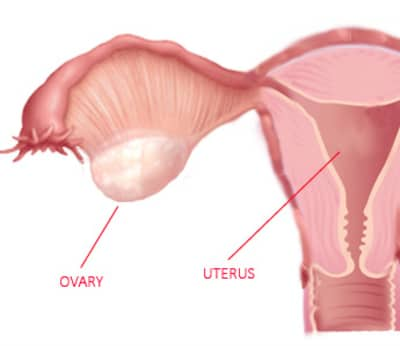
The ovaries, located on each side of a woman’s pelvis, are accountable for producing and launching eggs required for fertilization. It’s maybe not surprising, then, that the most typical causes of what individuals think about ovary pain, which is typically felt in the lower abdomen, pelvis, or lower back, are related to ovulation and menstruation. However, a gynecological issue like endometriosis or pelvic inflammatory disease, or perhaps a medical condition impacting your gastrointestinal or urinary system can be to blame. This can make the diagnosis difficult.
Causes of Ovary Pain on Left Side
It’s essential to learn about the variety of conditions that can be responsible for how you are feeling. Some may warrant your issue, while others may eliminate it.
Menstrual Pain
Women might experience pain or discomfort in one or both ovaries on certain days during a normal menstrual cycle. This cramping pain that a woman experiences during or simply prior to menstruation is called dysmenorrhea and is due to the release of prostaglandins — hormone-like compounds that, to name a few things, agreement muscles — from the uterus.
Mittelschmerz Pain
Some women experience ovarian pain mid-cycle during ovulation, when an egg is released from the ovary, instead of during menstruation. Referred to as mittelschmerz pain, it might be unpleasant however is safe.
Ovarian Cyst
An ovarian cyst is a benign growth, generally filled with fluid, that may cause pain, discomfort, bleeding, menstrual irregularities, or no symptoms at all. Ovarian cysts prevail and can develop at different points during the menstruation.
Follicular cysts are formed if an egg is not released during ovulation, and corpus luteum cysts establish if the corpus luteum (egg sac) does not dissolve as it must right after ovulation.
Small ovarian cysts may improve on their own, however some require immediate medical treatment, like a large cyst that bursts or bursts. This might cause abrupt, sharp, and extreme one-sided pelvic pain.
Endometriosis
Endometriosis is a condition in which the endometrial lining of the uterus can develop in other areas of a woman’s reproductive organs, like the ovaries, fallopian tubes, or on the bladder.
Endometriosis frequently causes extreme cyclical or episodic uterine or ovarian cramping pain and periodic bleeding. The pain may be especially extreme during a woman’s period or while having sex. Endometriosis might also result in infertility due to adhesion (scar tissue) formation.
Ectopic Pregnancy
An ectopic pregnancy is a pregnancy that occurs outside the uterus, normally in among the fallopian tubes. It might trigger moderate to severe ovarian pain and warrants first aid.
Pelvic Inflammatory Disease (PID)
PID is an infection that may affect one or more reproductive organs consisting of the uterus, ovaries, fallopian tubes, and vagina. This major condition is frequently triggered by a sexually transmitted infection and might lead to pain in numerous areas of the hips, consisting of one or both ovaries, that is frequently even worse with sex.
Besides pain, women with PID might experience fevers, chills, an abnormal vaginal discharge and/or bleeding, along with symptoms that imitate that of a urinary tract infection, like burning with urination.
Uterine Fibroids
Uterine fibroids are benign growths that emerge from the lining of the uterus. Besides pelvic discomfort or pressure, a woman with fibroids might experience abnormal uterine bleeding, back pain, constipation (if a fibroid is pressing on the bowel), urinary troubles (if the fibroid is continuing the bladder), and infertility.
Uncommon Causes
There are a couple of unusual conditions that may cause ovarian pain. Given the seriousness of the majority of these, it is essential not to neglect these symptoms, no matter the possibility of these issues.
Ovarian Cancer
Although ovarian cancer can trigger ovary pain, it is not common. In fact, the disease frequently does not cause any symptoms or, if it does, they are more subtle ones like bloating, feeling complete without eating much, and urinary seriousness or frequency.
Ovarian Remnant Syndrome
This is an uncommon condition that can result if you have had surgery to take out your ovaries and some tissue was not entirely removed. This could occur if you have endometriosis and there was a little area of endometrial or ovarian tissue that was not visualized throughout your surgery or that expanded after your treatment, for instance.
Ovarian Torsion
This is an unusual condition, but a surgical emergency in which one of the fallopian tubes ends up being twisted, potentially interrupting its blood supply and that of the ovary. This condition can trigger severe and unexpected pain due to ischemia (absence of blood flow) to these areas.
Phantom Ovary Pain
With phantom ovary pain, a woman continues to experience what appears like ovarian pain even after one or both of her ovaries has been gotten rid of. This is believed to be the result of persistent sensory nerve stimulation.
When to See a Doctor
You ought to see your doctor if you have new or various symptoms in the pelvic area, either with your period or in between periods.
More specifically, if you experience any of these symptoms, make certain to seek out healthcare:
- Consistent or extreme pelvic pain.
- Menstruations that are longer than 38 days or shorter than 24 days.
- Periods that last longer than seven days.
- Menstrual bleeding that soaks through several tampons or pads every hour for several hours in a row.
- Menstrual circulation with blood clots that are a quarter size or larger.
- Bleeding or spotting between periods.
- Bleeding after menopause.
- Bleeding during or after sex.
- Bleeding or constraining if you have actually missed out on a period or have tested favorable on a pregnancy test.
- Bleeding after menopause.
- Blood in your urine.
- Fevers, chills, night sweats, nausea, or throwing up.
Medical diagnosis
Identifying the cause of your ovary pain isn’t straightforward, as issues with other reproductive organs, like your uterus or cervix, and even other body systems might be at play. (The ovaries are located in the very same basic area as lots of other organs.).
If you see your doctor for ovarian pain, the first thing she will do is perform a medical history and physical examination.
Medical and Sexual History
Throughout your case history, your doctor will ask you a number of questions about your pain, like when it started, how it feels, what makes it much better and even worse, and whether or not you have other symptoms like vaginal bleeding, vaginal discharge, or fever.
She will also ask you whether you have actually ever been detected with a gynecological condition, such as endometriosis or uterine fibroids, and whether you have actually ever gone through abdominal or pelvic surgery prior to.
Physical exam
For ovarian pain, your medical professional will analyze your abdominal area and lower back and sides. In addition to inspecting and continuing these areas to look for inflammation, your medical professional will also carry out a pelvic exam.
During the pelvic exam, samples of your vaginal fluid or from your cervix might be taken by means of a Pap smear to assess for infection or abnormal cells.
Labs and Blood Tests
A range of tests may be ordered to confirm or discount a diagnosis, maybe the most crucial one being a pregnancy test to eliminate ectopic pregnancy.
Besides a pregnancy test, a urinalysis may be ordered to look for blood or an infection. Similarly, for PID, your physician might buy inflammatory blood markers, like C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR), or a complete blood count to look for a raised white blood cell count (a sign of infection).
Imaging
Due to the fact that there can be a variety of medical causes for your pain, do not be surprised if your physician orders imaging tests, such as a pelvic ultrasound or a computed tomography (CT) scan of your abdomen and pelvis.
Pelvic Laparoscopy
A pelvic laparoscopy is a surgery often used to identify what is triggering a woman’s pelvic pain. During a pelvic laparoscopy, your doctor might take a tissue sample (biopsy).
Differential Diagnoses
Gastrointestinal concerns, like constipation and even more major conditions, like appendicitis or diverticulitis, can lead to pain or discomfort that can be misinterpreted for ovarian pain.
If your physician presumes a gastrointestinal problem instead of a pelvic problem (for instance, if your pregnancy and pelvic test are normal, and your stomach examination reveals focal inflammation), she will proceed with suitable tests. For instance, a CT scan of the abdominal area can identify appendicitis and diverticulitis. Often, a clinical history and digital rectal test can detect constipation.
Likewise, a urinary tract infection (UTI) or kidney stone can trigger pain that feels like ovarian pain. These conditions can typically be eliminated fairly early with a normal urinalysis — that is, one that reveals no signs of infection and no proof of blood. A CT scan can be used to identify a kidney stone if one is still suspected.
Treatment
As soon as the “why” behind your ovary pain is determined, you and your doctor can move forward with designing a treatment plan that may be as easy as a couple of lifestyle changes to more included, like taking a prescription medication or undergoing surgery.
At Home Therapies
If your ovary pain is connected to your month-to-month cycle, lifestyle changes like getting sufficient sleep, working out, utilizing relaxation strategies, and using a heating pad can often help relieve your discomfort.
Medications
Depending upon your diagnosis, your physician may advise or recommend medication.
For instance, if simple home remedies like heat and rest are not easing your menstrual cramps, a nonsteroidal anti-inflammatory (NSAID) drug, which decreases the prostaglandin levels in your body, often helps. Make certain to speak with your doctor before taking an NSAID; women with bleeding disorders, an aspirin allergy, kidney or liver disease, or stomach problems need to not take these drugs. Besides NSAIDs, contraception approaches like the Pill, patch, ring, or the intrauterine device can also reduce menstrual cramps.
Another gynecological condition that requires medication is pelvic inflammatory disease. If identified with PID, your medical professional will recommend you antibiotics. In more extreme cases, a woman may need to be hospitalized and receive the antibiotics intravenously (through her vein).
Surgery
For emerging conditions, like ovarian torsion or ectopic pregnancy, surgery is called for. Surgery is likewise typically carried out as part of the treatment of ovarian cancer and may be used to get rid of uterine fibroids or endometrial tissue in severe endometriosis.

About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.