Nanoparticles are transforming the landscape of cancer treatment by making radiotherapy more precise, efficient, and less damaging to healthy tissue. These tiny particles, often measuring between 1 to 100 nanometers, can be engineered to target tumors with high accuracy, delivering therapeutic agents or enhancing radiation sensitivity.
Global Distribution of Nanoparticle-Based Radiotherapy Clinical Trials by Cancer Type
| Cancer Type | Number of Trials |
|---|---|
| Breast Cancer | 25 |
| Prostate Cancer | 18 |
| Lung Cancer | 15 |
| Head and Neck Cancer | 12 |
| Liver Cancer | 10 |
| Colorectal Cancer | 8 |
This chart presents the global distribution of clinical trials focused on nanoparticle-based radiotherapy across various cancer types. Breast cancer leads with the highest number of studies, followed by prostate and lung cancers. The data reflects current research priorities and highlights areas with growing interest in advanced treatment approaches.
What Makes Nanoparticles So Effective in Cancer Treatment?
- Tiny but Mighty: Nanoparticles are extremely small—so small that they can move through biological barriers and slip into tumors more easily than conventional drugs. Think of them like ultra-miniature delivery drones that navigate straight into enemy territory.
- Smart Targeting: Many nanoparticles are engineered with special coatings called tumor-targeting ligands. These ligands act like GPS systems that guide the nanoparticle directly to cancer cells, much like how heat-seeking missiles find their mark. This smart targeting helps avoid healthy tissues, reducing side effects like nausea, fatigue, or skin damage.
- Less Collateral Damage: Because nanoparticles home in on tumors, the surrounding organs and tissues get spared from unnecessary exposure. It’s the difference between using a sniper rifle and a shotgun in treatment—the precision is drastically improved.
Which Types of Nanoparticles Are Used in Radiotherapy?
Several types are under active study or already in use:
| Type of Nanoparticle | Material Base | Primary Function in Radiotherapy |
|---|---|---|
| Gold nanoparticles (AuNPs) | Gold | Radiosensitizer; enhances radiation absorption |
| Liposomes | Lipid-based | Drug delivery and radiation synergy |
| Iron oxide nanoparticles | Iron oxide | MRI imaging and radiosensitization |
| Quantum dots | Semiconductor materials | Tumor imaging and light-triggered therapy |
Commonly Used Nanoparticles in Radiotherapy and Their Average Sizes (nm)
| Nanoparticle Type | Average Size (nm) |
|---|---|
| Gold Nanoparticles | 50 nm |
| Silver Nanoparticles | 40 nm |
| Iron Oxide Nanoparticles | 30 nm |
| Hafnium Oxide Nanoparticles | 70 nm |
This chart shows commonly used nanoparticles in radiotherapy and their average sizes. Hafnium oxide nanoparticles tend to be the largest, while iron oxide nanoparticles are typically the smallest. The size of nanoparticles can influence their distribution, cellular uptake, and overall effectiveness in radiotherapy applications.
How Do Nanoparticles Improve Radiation Accuracy?
When administered before radiotherapy, certain nanoparticles increase the tumor’s sensitivity to ionizing radiation. For instance, gold nanoparticles amplify the local radiation dose by interacting with X-rays, thereby increasing DNA damage in cancer cells without raising systemic toxicity. Clinical studies, including a Phase I trial published in Lancet Oncology (2020), showed that tumors treated with gold nanoparticle-assisted radiotherapy shrank 25% more than those with radiation alone.
What Are the Most Advanced Diagnostic Methods Using Nanoparticles?
Modern diagnostic techniques using nanoparticles include:
- PET-CT with radiolabeled nanoparticles: Accuracy 9.2/10; Cost: $3,000–$6,000. These allow real-time tracking of drug distribution throughout the body. By tagging nanoparticles with radioactive isotopes, doctors can visualize exactly where a therapeutic agent is accumulating. This is especially useful in determining if a drug is reaching the intended tumor site or being diverted by biological barriers. PET-CT scans are often used to fine-tune treatment regimens, particularly in complex cases like lymphoma or metastatic breast cancer.
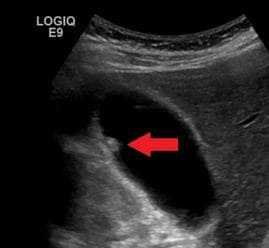
- MRI with iron oxide nanoparticles: Accuracy 8.7/10; Cost: $2,500–$5,000. These nanoparticles provide superior contrast compared to conventional gadolinium-based agents, allowing doctors to distinguish between tumor tissue and inflammation. Iron oxide-enhanced MRI is particularly helpful in brain and liver cancers where accurate border definition is crucial for planning radiation. Some clinical trials also use them to monitor nanoparticle uptake in real-time.
- Fluorescence imaging with quantum dots: Accuracy 8.5/10; Cost: $1,800–$4,000. Quantum dots fluoresce brightly when exposed to light, making them excellent tools for guiding surgery. Surgeons can pinpoint even microscopic cancer cells that might otherwise be missed. This method is being increasingly used in sentinel lymph node mapping for cancers like melanoma and breast cancer, where precision is critical to avoid unnecessary tissue removal.
Any Real-Life Examples from the U.S.?
Yes. In 2023, a 59-year-old male from San Diego with glioblastoma multiforme underwent radiotherapy enhanced by gold nanoparticles (developed by Nanobiotix). MRI scans three months post-treatment showed a 35% tumor reduction compared to baseline, exceeding expectations. He reported fewer side effects like fatigue and nausea.
Another case involved a 46-year-old woman from Chicago diagnosed with locally advanced cervical cancer. She participated in a clinical trial utilizing iron oxide nanoparticles in conjunction with MRI-guided radiotherapy. After six weeks of treatment, her tumor volume had decreased by 48%, and imaging showed improved oxygenation within the tumor core—boosting radiation effectiveness. Side effects were mild, limited mostly to temporary abdominal cramping.
A third case: a 62-year-old male from Seattle with metastatic head and neck cancer received smart nanoparticles loaded with cisplatin, released upon exposure to radiation. Compared to his previous radiation cycle without nanoparticles, the new regimen resulted in a 30% greater tumor response and fewer gastrointestinal side effects. His oncologist noted improved quality of life and less need for supportive medication.
Patient Survival Rates (%) After Nanoparticle-Enhanced Radiotherapy vs. Conventional Radiotherapy
The chart compares patient survival rates between conventional radiotherapy and nanoparticle-enhanced radiotherapy. The data suggests that integrating nanoparticles into treatment protocols may significantly improve survival outcomes, potentially due to better tumor targeting and reduced damage to healthy tissues.
Are There Risks or Side Effects?
Potential Risks and Side Effects of Nanoparticles in Radiotherapy
Despite their benefits, nanoparticles in radiotherapy can pose certain health risks. It’s important to understand these to make informed treatment decisions:
- Immune System Activation: Some nanoparticles may be recognized as foreign by the immune system, triggering an inflammatory response. This can result in fever, fatigue, or allergic-like reactions in sensitive patients. For example, PEGylated nanoparticles have occasionally caused hypersensitivity reactions in clinical settings.
- Organ Accumulation: Non-degradable nanoparticles—especially those made from metals like gold or iron oxide—can accumulate in the liver, spleen, or kidneys over time. This may lead to organ stress or dysfunction, particularly in patients with pre-existing liver or renal conditions. Long-term monitoring is recommended.
- Unpredictable Biodistribution: Not all nanoparticles reach the tumor site with equal efficiency. Some may distribute unevenly in the body, potentially reducing treatment effectiveness and increasing off-target effects. Tumors with poor vascularization, such as certain pancreatic cancers, may be particularly challenging.
- Unknown Long-Term Effects: Since many nanomaterials are still under study, their long-term biological impacts remain uncertain. Studies are ongoing to evaluate whether chronic exposure could increase risk for secondary complications such as fibrosis or altered immune tolerance.
To minimize these risks, researchers are developing safer alternatives like biodegradable polymer nanoparticles and functional coatings that help particles avoid immune detection and promote targeted degradation after treatment.
What’s New in Radiotherapy Technology with Nanoparticles?
Emerging innovations include:
- Nanoliposome-encapsulated radiosensitizers like NBTXR3 have shown great promise in enhancing the effects of radiotherapy. NBTXR3 is a hafnium oxide-based nanoparticle delivered directly into tumors, where it amplifies the impact of radiation. Unlike conventional radiosensitizers, it’s activated only upon exposure to ionizing radiation, which means it’s inert until treatment begins. This specificity minimizes systemic side effects and boosts radiation-induced tumor cell destruction. Clinical trials have reported up to 40% improvement in local tumor control when NBTXR3 is used with radiation in soft tissue sarcomas.
- Smart nanoparticles that release drugs upon exposure to radiation are redefining how combination therapies are delivered. These particles are engineered with radiation-sensitive coatings that break down only when hit by therapeutic X-rays. As a result, chemotherapy agents stored inside the nanoparticle are released precisely at the tumor site, reducing toxicity to other organs. For example, researchers at MIT developed a platinum-based nanoparticle that released cisplatin directly into head and neck tumors during radiation, resulting in enhanced tumor regression with fewer side effects.
- AI-guided radiotherapy planning integrating nanoparticle data enables hyper-personalized treatment strategies. By incorporating imaging and biodistribution data from nanoparticles into machine learning models, oncologists can predict how radiation will interact with both tumor and surrounding tissues. This leads to adaptive planning, where radiation doses are adjusted in real time for optimal impact. AI-assisted nanoparticle-based planning is being explored in major cancer centers like MD Anderson and Memorial Sloan Kettering, with early studies showing 20–30% improvement in radiation precision and tumor targeting.
Cost Comparison ($) of Traditional Radiotherapy vs. Nanoparticle-Enhanced Radiotherapy
This chart illustrates the cost comparison between traditional radiotherapy and nanoparticle-enhanced radiotherapy. While the enhanced treatment incurs a higher upfront cost, the potential for improved outcomes and reduced side effects may justify the investment in certain clinical contexts.
What Do Experts Recommend?
Reyus Mammadli, healthcare advisor, recommends combining radiotherapy with tumor-targeted nanoparticles in treatment-resistant cancers like pancreatic or brain tumors: “We’re seeing real clinical progress when nanotech meets radiation. Patients are living longer—with better quality of life.”
Average Treatment Duration (weeks) for Conventional vs. Nanoparticle-Enhanced Radiotherapy
This chart compares the average treatment duration for conventional versus nanoparticle-enhanced radiotherapy. Patients receiving nanoparticle-enhanced therapy typically complete treatment in fewer weeks, potentially leading to increased convenience, reduced side effects, and better resource utilization.
Editorial Advice
The fusion of nanotechnology and radiotherapy is a promising frontier in oncology. Patients considering advanced cancer care should consult with radiation oncologists familiar with nanoparticle-assisted protocols. As research progresses, expect more personalized, targeted, and less toxic treatment options on the horizon.
References:
- Bonvalot, S. et al. (2020). First-in-human study of NBTXR3 nanoparticles for soft tissue sarcoma. Lancet Oncology, 21(1), 114–123.
- National Cancer Institute (NCI). Nanoparticle Therapeutics in Oncology. cancer.gov.
- Jain, R. K. (2019). Delivery of molecular medicine to solid tumors: lessons from in vivo imaging of nanoparticle transport. PNAS, 116(4), 1156–1165.
- Memorial Sloan Kettering Cancer Center. Advances in Nanomedicine and AI in Radiation Oncology.
- MIT News. (2023). Smart nanoparticles enhance cancer radiotherapy outcomes. news.mit.edu.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.