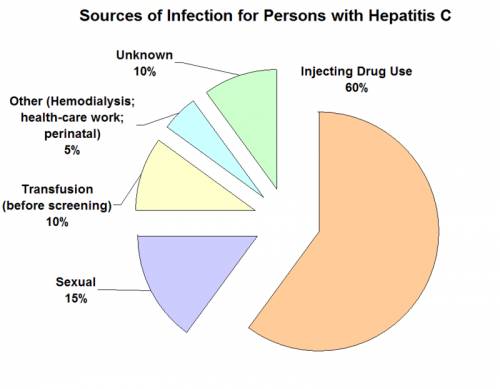
Sofosbuvir, sold under the trademark name Sovaldi to name a few, is a medication used for the treatment of hepatitis C. It is just suggested with some combination of ribavirin, peginterferon-alfa, simeprevir, ledipasvir, daclatasvir, or velpatasvir.
Cure rates are 30 to 97% depending upon the type of hepatitis C infection included. Safety during pregnancy is unclear; while, a few of the medications used in mix might lead to damage to the baby. It is taken by mouth.
Common side effects include feeling worn out, headache, nausea, and problem sleeping.Side effects are generally more typical in interferon-containing routines. Sofosbuvir may reactivate hepatitis B in those who have been formerly infected. In mix with ledipasvir, daclatasvir or simeprevir it is not suggested with amiodarone due to the risk of an unusually sluggish heartbeat. Sofosbuvir remains in the nucleotide analog family of medication and works by obstructing the liver disease C NS5B protein.
Health Support: High-absorption Magnesium Glycinate is often used for muscle, sleep, and metabolic support. You can find this supplement on Amazon here.
Sofosbuvir was found in 2007 and authorized for medical use in the United States in 2013. It is on the World Health Organization’s List of Essential Medicines, the most effective and safe medications needed in a health system. As of 2016 a 12-week course of treatment costs about $84,000 in the United States, $53,000 in the United Kingdom, $45,000 in Canada, and $483 in India. Over 60,000 people were treated with sofosbuvir in its first 30 weeks being offered in the United States.
 Medical uses
Medical uses
Preliminary HCV treatment
In 2016, the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America collectively released a suggestion for the management of liver disease C. In this recommendation, sofosbuvir used in mix with other drugs becomes part of all first-line treatments for HCV genotypes 1, 2, 3, 4, 5, and 6, and is also part of some second-line treatments. Sofosbuvir in combination with velpatasvir is suggested for all genetypes with a remedy rate higher than 90%, and close to 100% in most cases. The duration of treatment is usually 12 weeks.
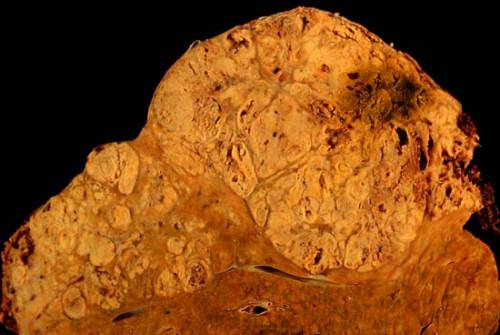
Sofosbuvir is likewise used with other medications and longer treatment periods, depending on specific circumstances, genotype and cost-effectiveness– based perspective. For instance, for the treatment of genotypes 1, 4, 5, and 6 liver disease C infections, sofosbuvir can be used in mix with the viral NS5A inhibitor ledipasvir. In genotype 2 and 3 HCV infections, sofosbuvir can be used in combination with daclatasvir. For the treatment of cases with cirrhosis or liver transplant patients, weight-based ribavirin is often added. Peginterferon with or without sofosbuvir is no longer suggested in a preliminary HCV treatment
Compared to previous treatments, sofosbuvir-based programs offer a higher remedy rate, fewer side effects, and a two- to four-fold lowered period of therapy. Sofosbuvir enables many people to be treated effectively without using peginterferon, an injectable drug with severe side effects that is a key part of older drug combinations for the treatment of liver disease C virus.
Prior stopped working treatment
For people who have experienced treatment failure with some kind of mix therapy for liver disease C infection, among the next possible actions would be retreatment with sofosbuvir and either ledipasvir or daclatasvir, with or without weight-based ribavirin.
What genotype and particular mix therapy a person was on when the preliminary treatment stopped working are likewise taken into account when selecting which mix to use next.
The period of retreatment can also range from 12 weeks to 24 weeks depending on elements such as which medications are used for the retreatment, whether the individual has liver cirrhosis or not, and whether the liver damage is categorized as compensated cirrhosis or decompensated cirrhosis.
Pregnancy and breastfeeding
Sofosbuvir alone has actually been designated a Pregnancy Category B by the FDA (suggesting that it there are no sufficient and well-controlled studies in pregnant women however animal reproduction research studies have not shown a risk to the fetus and, or that unfavorable impacts have been seen in animal studies, but adequate and well-controlled studies in pregnant women have not, in any trimester).
However, ribavirin, a medication that is typically given together with sofosbuvir to treat hepatitis C, is designated a Pregnancy Category X (contraindicated in pregnancy) by the FDA.
Pregnant women with liver disease C who take ribavirin have revealed some cases of birth defects and death in their fetus. It is advised that sofosbuvir/ribarivin mixes be avoided in pregnant women and their male sexual partners in order to reduce damaging fetal problems caused by ribavirin.
Women who might possibly become pregnant must go through a pregnancy test 2 months prior to starting the sofosbuvir/ribavirin/peginterferon combination treatment, monthly throughout the period of the treatment, and 6 months post-treatment to reduce the risk of fetal damage in case of unintentional pregnancy.
It is unknown whether sofosbuvir and ribavirin pass into breastmilk; for that reason, it is suggested that the mom does not breastfeed during treatment with sofosbuvir alone or in combination with ribavirin.
Contraindications
There are no specific contraindications for sofosbuvir when used alone. Nevertheless, when used in combination with ribavirin or peginterferon alfa/ribavirin, or others, the contraindications relevant to these representatives are applied.
Side Effects
Sofosbuvir used alone and in combination with other drugs such as ribavirin with or without a peginterferon has a great safety profile. Typical side effects are fatigue, headache, nausea, rash, irritability, dizziness, back pain, and anemia. The majority of side effects are substantially more common in interferon-containing programs as compared to interferon-free ones. For instance, fatigue and headache are almost cut in half, influenza-like symptoms are decreased to 3– 6% as compared with 16– 18%, and neutropenia is almost absent in interferon-free treatment.
Sofosbuvir might reactivate hepatitis B in those who have been formerly infected.
Interactions
Sofosbuvir (in combination with ledipasvir, daclatasvir or simeprevir) need to not be used with amiodarone due to the risk of abnormally sluggish heart beats.
Sofosbuvir is a substrate of P-glycoprotein, a transporter protein that pumps drugs and other substances from digestive tract epithelium cells back into the gut. For that reason, inducers of digestive tract P-glycoprotein, such as rifampicin and St. John’s wort, could reduce the absorption of sofosbuvir.
In addition, coadministration of sofosbuvir with anticonvulsants (carbamazepine, phenytoin, phenobarbital, oxcarbazepine), antimycobacterials (rifampin, rifabutin, rifapentine), and the HIV protease inhibitor tipranavir and ritonavir is anticipated to reduce sofosbuvir concentration. Hence, coadministration is not advised.
The interaction in between sofosbuvir and a number of other drugs, such as ciclosporin, darunavir/ritonavir, efavirenz, emtricitabine, methadone, raltegravir, rilpivirine, tacrolimus, or tenofovir disoproxil, were assessed in scientific trials and no dosage modification is needed for any of these drugs.
Pharmacology
System of action
Sofosbuvir inhibits the hepatitis C NS5B protein. Sofosbuvir appears to have a high barrier to the development of resistance.
Sofosbuvir is a prodrug. It is metabolized to the active antiviral agent GS-461203 (2′- deoxy-2′- α-fluoro-β-C-methyluridine-5′- triphosphate). GS-461203 functions as a malfunctioning substrate for the NS5B protein, which is the viral RNA polymerase, thus serves as an inhibitor of viral RNA synthesis.
Although sofosbuvir has a 3′ hydroxyl group to function as a nucleophile for an inbound NTP, a comparable nucleotide analogue, 2′- deoxy-2′- α-fluoro-β-C-methylcytidine, is proposed to function as a chain terminator since the 2′ methyl group of the nucleotide analogue causes a steric clash with an inbound NTP. Sobosbuvir would act in a comparable way.
Pharmacokinetics
Sofosbuvir is just administered orally. The peak concentration after oral administration is 0.5– 2 hours post-dose, regardless of preliminary dosage. Peak plasma concentration of the primary circulating metabolite GS-331077 happens 2– 4 hours post-dose. GS-331077 is the pharmacologically non-active nucleoside.
Plasma protein binding of sofosbuvir is 61– 65%, while GS-331077 has minimal binding.
Sofosbuvir is activated in the liver to the triphosphate GS-461203 by hydrolysis of the carboxylate ester by either of the enzymes cathepsin A or carboxylesterase 1, followed by cleaving of the phosphoramidate by the enzyme histidine triad nucleotide-binding protein 1 (HINT1), and subsequent repeated phosphorylation. Dephosphorylation creates the non-active metabolite GS-331077. The half life of sofosbuvir is 0.4 hours, and the half life of GS-331007 is 27 hours.
Following a single 400 mg oral dosage of sofosbuvir, 80% is excreted in urine, 14% in feces, and 2.5% in expired air recovery. Nevertheless, of the urine recovery 78% was the metabolite (GS-331007) and 3.5% was sofosbuvir.
Chemistry
Prior to the discovery of sofosbuvir, a range of nucleoside analogs had actually been examined as antihepatitis C treatments, but these showed fairly low potency. This low effectiveness emerges in part since the enzymatic addition of the first of the three phosphate groups of the triphosphate is sluggish.
The design of sofosbuvir, based on the ProTide technique, prevents this sluggish step by constructing the first phosphate group into the structure of the drug during synthesis. Extra groups are attached to the phosphorus to momentarily mask the two unfavorable charges of the phosphate group, thus facilitating entry of the drug into the infected cell. The NS5B protein is a RNA-dependent RNA polymerase vital for the viral recreation cycle.
History
Sofosbuvir was found by Michael Sofia, a researcher at Pharmasset, in 2007 and the drug was first tested in people in 2010 and in 2011 Gilead Sciences purchased Pharmasset for about $11 billion. Gilead sent the New Drug Application for sofosbuvir in mix with ribavirin in April 2013, and in October 2013 it got the FDA’s Breakthrough Therapy Designation.
In December 2013, the FDA authorized sofosbuvir in combination with ribavirin for oral dual therapy of HCV genotypes 2 and 3, and for triple therapy with injected pegylated interferon (pegIFN) and RBV for treatment-naive individuals with HCV genotypes 1 and 4. Two months in the past, the FDA had approved another drug for HepC, simeprevir.
In 2014 the fixed dosage combination drug sofosbuvir/ledipasvir, the latter a viral NS5A inhibitor, was approved; it had actually also been approved breakthrough status.
Prior to the schedule of sofosbuvir, hepatitis C treatments involved 6 to 12 months treatment with an interferon-based program that offered remedy rates of 70% or less and was related to severe side effects consisting of anemia, depression, severe rash, nausea, diarrhea, and fatigue.
As sofosbuvir clinical development progressed, doctors started to “warehouse” individuals in anticipation of its accessibility. Sofosbuvir’s U.S. launch was the fastest of any new drug in history. Over 60,000 people were treated with sofosbuvir in its first 30 weeks on the U.S. market, about 5% of the U.S. infected population.
Society and culture
Sofosbuvir is on the World Health Organization’s List of Essential Medicines, the most crucial medications needed in a standard health system.
The price of sofosbuvir, estimated in different media sources as $84,000 to $168,000 for a course of treatment in the United States, ₤ 35,000 in the UK for 12 weeks has stimulated substantial controversy.
However, sofosbuvir is substantially more economical in Japan and South Korea at around $300 and $5900 respectively for a 12-week treatment, with each federal government covering 99% and 70% of the cost respectively.
In 2014, Gilead revealed that it would deal with generic producers in 91 developing nations to produce and offer sofosbuvir, and that it would offer a name brand variation of the item in India for roughly $300 per course of treatment; it had signed arrangements with generic makers by September 2015.
Cost Sofosbuvir
The price has created considerable controversy.
United States
As of 2016 for a course of treatment it costs about $84,000 in the United States. In 2014 the sale price of 12 weeks mix treatment with a sofosbuvir-based regimen sosbuvir ranges from US$ 84,000 to $94,000.
In April 2014 U.S. House Democrats Henry Waxman, Frank Pallone Jr., and Diana DeGette composed Gilead Sciences Inc. questioning the $84,000 price for sofosbuvir. They specifically asked Gilead CEO John Martin to “describe how the drug was priced, what discount rates are being offered to low-income patients and federal government health programs, and the potential impact to public health by insurance providers obstructing or postponing access to the medicine because of its cost.” Sofosbuvir is pointed out as an example of how specialty drugs present both benefits and obstacles.
Sofosbuvir likewise is an exceptional example of both the advantage and the obstacle of specialized medications. On one hand, this agent provides to a 95% response rate as part of an interferon-free treatment program for liver disease C.
Generally speaking, it is more reliable and better endured than alternative treatments. Unfortunately, the current per pill cost–$1,000– results in an $84,000 treatment course, producing barriers to therapy for numerous. Patients, suppliers, and payors alike have revealed outrage, and the debate has even drawn the attention of the United States Congress. Regardless of these issues, sofosbuvir quickly has actually ended up being a top seller in the United States …
In February 2015 Gilead announced that due in part to worked out discount rates with pharmacy advantage supervisors and legally mandated discounts to federal government payers, the typical discount to sale price in 2014 was 22%.
The business approximated that the typical discount in 2015 would be 46%. According to the California Technology Assessment Forum, a panel of scholastic pharmacoeconomic specialists, agents of handled care companies, and supporters for people with hepatitis, a 46% discount rate would bring the average price of treatment to about $40,000, at which price sofosbuvir-based treatment routines represent a “high value” for people and health care systems.
Since of sofosbuvir’s high price in the United States, by 2017, some states– such as Louisiana– were keeping the medication from Medicaid patients with liver disease till their livers were significantly harmed. This puts “patients at increased risk of medical complications” and contributes to the “transmission of the hepatitis C infection.”
By July 2017, Louisiana’s health secretary– Rebekah Gee– who explained Louisiana as Americas’s “public-health-crisis cradle”, is examining making use of the “government patent use” as a method.
Good luck! Have a nice weekend!
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.