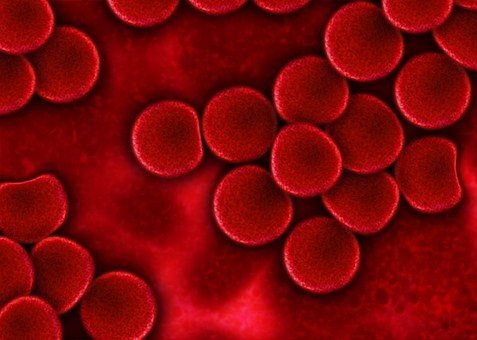
Anemia indicates “bloodlessness” in Latin. That’s due to the fact that it lowers the number of red blood cells made in bone marrow. Red blood cells bring oxygen throughout the body, so with fewer of them, the body ends up being starved for oxygen.
Anemia also can lead to bone marrow making insufficient quantities of hemoglobin. Hemoglobin is an iron-rich protein that enables red blood cells to bring oxygen through the blood. Anemia is seldom life-threatening, however, certain types of anemia can be deadly if left untreated.
What Are the Different Kinds of Anemia?
There are a number of types of anemia, and each type has a various cause. For example, pernicious anemia is caused by an absence of vitamin B12 in the body. Iron shortage anemia is caused by an absence of iron, which bone marrow has to make hemoglobin.
Other types of anemia include sickle cell anemia, vitamin shortage anemia, anemia related to bone marrow disease, and aplastic anemia. Some sort of anemia can be cured easily, while others can not. Some may be harmful.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis is an autoimmune, systemic disease that affects the joints. In rheumatoid arthritis (early signs), the body’s immune system errors the body’s tissue for a foreign intruder. This leads the immune system to attack the protective cushion of tissue and fluid in between the joints. The result is swelling, tightness, and pain in the joint.
The body’s misfiring immune system also may pursue the body’s soft tissues, like cartilage, and organs such as the heart, eyes, and veins. Ultimately, rheumatoid arthritis can cause long-term damage, disability, and anemia.
Link Between Rheumatoid Arthritis and Anemia
One type of anemia accompanies chronic inflammatory diseases, such as rheumatoid arthritis. Rheumatoid arthritis can be connected with other types of anemia, consisting of aplastic anemia and iron deficiency anemia.
When rheumatoid arthritis is active, the autoimmune reaction causes inflammation in the joints and other tissues. Inflammation lowers the production of red blood cells by triggering a release of specific proteins that impact how the body uses iron.
Inflammation may likewise impact the way the body produces erythropoietin, a hormone that controls the production of red blood cells.
Can Rheumatoid Arthritis Drugs Cause Anemia?
Simply put, yes. Non-steroidal anti-inflammatory drugs (NSAIDs) such as acetaminophen, naproxen, and ibuprofen can cause bleeding ulcers to form in the stomach or digestive tract. This causes blood loss, which results in anemia. It can be treated with blood infusions to recover the ulcers.
NSAIDs, particularly acetaminophen (Tylenol) can also damage the liver, where iron from the foods you eat is saved and launched for later use. Disease-modifying antirheumatic drugs (DMARDs) including biologics likewise can cause liver damage and anemia.
If you take rheumatoid arthritis drugs, your doctor will need frequent blood tests.
Symptoms of Anemia
Anemia symptoms and signs differ depending upon the cause of your anemia. They may include:
- Tiredness
- Weakness
- Pale or yellow-colored skin
- Irregular heartbeats
- Shortness of breath
- Dizziness or lightheadedness
- Chest pain
- Cold hands and feet
- Headache
At first anemia can be so mild that it goes undetected. But symptoms intensify as anemia worsens.
When to see a doctor
Make a visit with your doctor if you’re feeling fatigued for unusual reasons. Some anemias, such as iron shortage anemia or vitamin B-12 shortage, are common.
Fatigue has lots of causes besides anemia, so do not presume that if you’re tired you should be anemic. Some people discover that their hemoglobin is low, which shows anemia, when they go to donate blood. If you’re informed that you can’t contribute blood because of low hemoglobin, make an appointment with your doctor.
How Is Anemia Diagnosed?
Your doctor will go over anemia symptoms with you. Possible symptoms include:
- weakness
- shortness of breath
- tiredness
- headaches
- pale skin
- cold hands or feet
- chest pain (as your heart is forced to work harder to pump oxygenated blood through your body).

Rheumatoid arthritis-related anemia is often mild enough that you do not feel any symptoms. Because case, blood tests can determine its presence. Blood tests likewise verify a diagnosis of anemia when symptoms are present.
What Tests Are Used to Diagnose Anemia?
Your doctor will do a physical examination in order to make an anemia diagnosis. They’ll listen to your heart and lungs and might continue your abdomen to feel the size and shape of your liver and spleen.
Doctors also use blood tests to make a diagnosis. These tests include:
- hemoglobin level test
- red cell count
- reticulocyte count (procedures the number of immature red blood cells you have)
- serum ferritin (steps the amount of this iron-storing protein)
- serum iron (procedures how much iron remains in your blood).
How Is Anemia Treated?
As soon as your doctor understands the cause of your anemia, they can begin treating it. Sometimes, individuals do not need any treatment. One method to treat rheumatoid arthritis-related anemia is to straight treat rheumatoid arthritis by decreasing inflammation in your body.
Patients with low iron levels might benefit from iron supplements. Nevertheless, excessive iron can develop other serious medical problems.
Though it’s hardly ever used, a drug called erythropoietin stimulates the blood marrow to produce more red blood cells.
Diet for Anemia
Iron supplements and foods abundant in iron are should in patient struggling with anemia. Heme Iron present in animal sources like beef liver, oysters, shrimp are most advised.
Iron Rich Foods
Anemic patient diet ought to be filled with iron content. Sources are turkey, chicken liver which fall under the classification of Heme Iron.
Anemia Nutrition
Iron-deficiency anemia diet must also consist of green leafy veggies like broccoli, collards, turnip green. Iron rich supplements can also be taken however they impose risk of abdominal area irritation.
Good luck! Have a nice weekend.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.