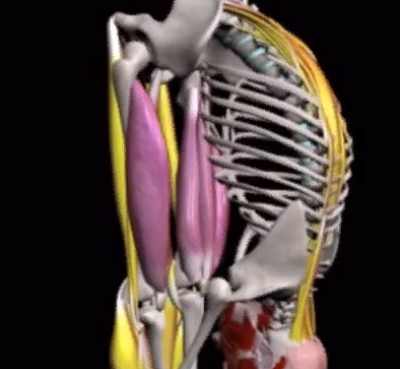
What is thigh pain? Thigh pain is any type of pain or discomfort impacting the area extending from the hips to the knee. Your thighs provide structural assistance and make it possible for motion, and are comprised of bones, muscles, tendons, ligaments, nerves, and blood vessels.
Thigh muscles provide movement and tendons anchor your thigh muscles to the bones of the pelvis and lower leg. Ligaments hold the thigh bone (femur) together with the pelvis and the lower leg bones to create the hip and knee joints. Nerves control feeling and movement, and capillary make sure constant blood flow to and from the thighs. Any of the structures of the thighs undergo injury, infection, diseases, or other conditions that can produce pain.
Thigh pain
Thigh pain can develop unexpectedly or slowly. Thigh pain may feel dull and throbbing, throbbing, piercing, or tingling. You may likewise experience paresthesias, pain-like feelings typically described as pins and needles or burning. Thigh pain might be just irritating and unpleasant or be so devastating that you can not put weight on your leg or walk.
Indeed, affection of the soft tissues around the joint is the most common cause of hip pain. Typically, such cases are diagnosed with trochanteritis – inflammation at the attachment of the tendon of the so-called femoral-tibial tract to the greater trochanter of the femur (in Latin, trochanter is trochanter, hence trochanteritis).
Trochanteritis usually manifests itself by pain on the lateral surface of the hip, with a maximum in the most protruding part (this is where patients “feel” their hip joint, although in reality the hip joint is in the groin area). It hurts when straining: climbing stairs, walking for a long time, but most often when lying on the side.
The triggering factor is the same type of load on the hip, combined with hypotrophy of the ligamentous and muscular apparatus (hi gymnastics!). It is treated by the administration of analgesic measures (local injections, oral medications) and the selection of adequate physical activity. But ointments are ineffective: a sufficiently large fat and muscle layer does not allow their penetration to the center of inflammation.
Rarely, patients are faced with the true lesion of the hip joint, among the causes of which the first place belongs to osteoarthritis. This is a degenerative disease characterized by the affection of all structures of the joint, but the main factor is the “thinning” of articular cartilage. This gradually leads to the “convergence” of bone surfaces with each other, the occurrence of pain and limitation of movement in the joint.
Pain in osteoarthritis of the hip joint is usually localized in the groin area, can extend to the buttock and increases with strain. Often the first symptom is pain in the knee joint, because when loading the injured hip joint, the pain is reflected in the completely intact knee joint.
What other symptoms might accompany thigh pain?
Thigh pain can establish together with other symptoms, which vary depending on the underlying disease, condition or condition. Additional symptoms can include other body systems or areas, such as the cardiovascular and neurological systems. Other symptoms that might accompany thigh pain consist of:
- Bleeding.
- Bruising, laceration or abrasion.
- Burning or prickling sensation.
- Change in gait such as hopping.
- Flu-like symptoms (tiredness, fever, sore throat, headache, cough, aches and pains).
- Joint pain.
- Muscle convulsions.
- Minimized variety of movement.
- Swelling.
- Tingling, pain, or other abnormal feelings in the toes.
Symptoms that might suggest a major or life-threatening condition
In many cases, thigh pain may occur with other symptoms that might indicate a severe or dangerous condition, such as deep vein apoplexy, which is a blood clot in the leg that can take a trip to the lungs and cause a deadly lung embolism. Other severe conditions include a fracture or infection. Seek immediate medical care (call 911) if you, or someone you are with, have other major symptoms, with or without thigh pain, including:
- Modification in consciousness or alertness such as fainting.
- Chest pain.
- Problem breathing, wheezing, or shortness of breath.
- Discolored, uncommonly light, or cold leg.
- Failure to walk or put weight on your leg.
- Popping sound sometimes of injury.
- Red, warm and swollen calf or leg.
- Severe pain.
- Severe swelling or deformity of the knee, thigh or hip.
What causes thigh pain?
There are a variety of conditions that can cause thigh pain. For instance, thigh pain can be brought on by exercise, injury, or age-related wear and tear on the hips and knees, which may cause pain or pain in the thigh area near the joint. Thigh pain can likewise be triggered by infections along with illness and conditions that affect numerous body systems or areas, such as diabetes or peripheral artery disease (PAD).
Injury and injury-related causes of thigh pain.
Thigh pain may be triggered by injuries and other trauma including:
- Bone fracture (damaged bone) or dislocation, particularly of the hip or thigh bone (thigh).
- Groin pull or strain.
- Laceration, abrasion or contusion of the thigh.
- Ligament sprains and tears, particularly of the anterior cruciate ligament (ACL) and medial security ligament (MCL) of the knees, which ensure leg and knee stability. Sprains and tears may cause pain or pain in the thigh area near the joint.
- Meniscus tear (tear in the shock-absorbing cartilage of the knee).
- Muscle cramp (charley horse), typically triggered by dehydration or overuse.
- Stretched or pulled thigh muscles, such as a hamstring or quadriceps muscle strain.
- Tendinitis (inflammation or irritation of tendons due to overuse or injury).
Transmittable causes of thigh pain
Thigh pain can be caused by different infections consisting of:
- Cellulitis (invasive infection of the skin and surrounding tissues).
- Infection of an injury or sore.
- Infection of the knee or hip, which can lead to septic arthritis and trigger pain in the joint that radiates to the thigh area.
- Osteomyelitis (bone infection).
Neurological causes of thigh pain
Thigh pain can be triggered by neurological conditions that trigger inflammation, entrapment, compression, or damage to the nerves including:
- Peripheral neuropathy (condition that causes damage and dysfunction of nerves that lie outside your brain and spine) and diabetic neuropathy (neuropathy caused by long-lasting diabetes).
- Piriformis syndrome (buttock muscle compressing or aggravating the sciatic nerve that causes pain, tingling or numbness down the leg).
- Sciatica (compression, injury or swelling of the sciatic nerve that causes burning or shooting pain ranging from the butts down the back of the leg).
Other causes of thigh pain
Thigh pain can be due to other causes including:
- Compartment syndrome (pressure within muscles constructs to unsafe levels, minimizing important blood flow to nerve and muscle cells).
- Deep vein thrombosis (blood clot in the leg that can break out from the leg, causing a pulmonary embolism in the lung, a cardiovascular disease, or stroke).
- Fibromyalgia (persistent condition triggering extensive muscular pain, tightness and inflammation).
- Peripheral artery disease (PAD, likewise called peripheral vascular disease, or PVD, which is a constricting of arteries due to an accumulation of fat and cholesterol on the walls of arteries, which limits blood circulation to the extremities).
- Restless legs syndrome (RLS; a movement condition identified by a powerful desire to move your legs, particularly when resting or sitting).
- Varicose veins.
The first movement that becomes difficult with osteoarthritis is abduction: it can be easily checked by trying to do the “frog” or sitting in the “lotus position,” and in everyday life the patient has problems putting on socks and shoes. Later on, patients begin to have difficulty with other movements as well, such as bending and adduction.
A common misconception among patients is that osteoarthritis is the province of older women. First of all, the incidence of hip arthritis in men and women is equal, and secondly, there is secondary osteoarthritis, which develops on the background of other joint pathology. This can be dysplasia (developmental disorder), coxitis (inflammation), aseptic necrosis of the femoral head (disruption of the blood supply to the bone tissue with its subsequent destruction), more typical for young patients.
In addition to the above, the pain in the hip can be caused by compression of the spinal nerve roots (e.g. herniated disc in the lumbar spine), femoroacetabular impingement syndrome, multiple arthritis involving the hip joints, and systemic connective tissue diseases such as rheumatic polymyalgia.
In all of these cases, diagnosis and therapy will vary: from simple examination to MRI and specific laboratory values, from prescription of gymnastics to referral for surgical treatment or therapy with cytostatics, from a single visit to the need for lifelong follow-up.
Key to all of these issues is the quality of the interview and examination. Therefore, before you go to the doctor, collect and organize information about all existing diseases, lay out in chronological order the laboratory and instrumental examinations, write down your complaints and questions to the doctor. This way you will help the specialist to understand your problem and prescribe an effective therapy.
Possible causes of hip pain at night and why your hip hurts during the day:
In addition to osteoarthritis and arthritis of various origins, trauma and fractures, among the myriad causes of hip pain are:
- Bursitis, tendonitis and inflammation of the soft tissue surrounding and articulating the femoral head and acetabulum;
- anglizing spondyloarthritis (an inflammatory rheumatic disease based on genetics that affects the sacral tract of the spine, causing bone changes and pain that radiates down the buttocks and leg)
- Arthritis associated with chronic inflammatory bowel disease (e.g., ulcerative colitis and Crohn’s disease);
- inflammation of the sciatic nerve (especially if it also involves nerves that start from the lumbar vertebrae toward the pelvis and legs)
- inflammation of the lateral femoral nerve (often in pregnancy, in persons with diabetes, and in those who regularly wear very tight clothing in the pelvis and hips);
- the presence of an inguinal or femoral hernia;
- fibromyalgia (a syndrome characterized by widespread muscle pain, cramps, sleep disturbances, and severe fatigue);
- inflammation and viral or bacterial infections of the hip joint;
- sickle cell anemia (a severe form of hereditary anemia in which the red blood cells take on a sickle shape);
- necrosis of the femoral head (degeneration of the bone and surrounding structures, which can occur due to altered vascularization, as a result of improper fracture/dislocation disruption, or even as an adverse event of certain therapies, such as radiation therapy, in the pelvis or taking high-dose corticosteroids, in childhood, is a major manifestation of Perthes disease)
- The presence of a primary or metastatic bone neoplasm.
- It should be noted that if pain in the thigh depends on diseases not primarily related to the joints or involving other organs or apparatuses, there are usually other more or less specific symptoms as well.
What are the prospective issues of thigh pain?
Issues of thigh pain can vary depending upon the underlying cause. Pain due to a minor condition, such as a moderate muscle strain or contusion, usually responds to rest, ice, and non-prescription anti-inflammatory medications. Nevertheless, some underlying causes of thigh pain, such as diabetic neuropathy and peripheral artery disease, can cause serious and potentially dangerous complications consisting of:
- Chronic pain.
- Trouble walking.
- Disability.
- Loss of hip or knee joint movement.
- Permanent nerve damage.
- Poor quality of life.
- Pulmonary embolism related to deep vein apoplexy.
- Spread of infection and major infections, such as gangrene, which can cause amputation.
- Weak point or paralysis.
It is very important to call your health care service provider when you have persistent pain or other unusual symptoms. Once the underlying cause is identified, following the treatment strategy described by your health care provider can decrease your risk of issues.
Treatment
Many cramps can be stopped if the muscle can be extended. For lots of cramps of the feet and legs, this stretching can typically be accomplished by standing and walking around. For a calf muscle cramp, the individual can stand about 2 to 2.5 feet from a wall (potentially further for a tall person) and lean into the wall to place the lower arms versus the wall with the knees and back straight and the heels in contact with the floor. (It is best to learn this maneuver at a time when you don’t have the cramp).
Another method includes bending the ankle by pulling the toes up toward the head while still lying in bed with the leg as straight as possible. For writer’s cramp (contractures in the hand), pressing the hand on a wall with the fingers facing down will extend the cramping finger flexor muscles.
Carefully massaging the muscle will typically help it to unwind, as will applying warmth from a heating pad or hot soak. If the cramp is associated with fluid loss, as is typically the case with vigorous physical activity, fluid and electrolyte (specifically sodium and potassium) replacement is vital. Medicines usually are not had to treat a regular cramp that is active since a lot of cramps go away spontaneously in the past adequate medicine would be taken in to even have an impact.
9 Ways to Relieve Thigh Pain
Effective tips for eliminating discomfort:
- Start your day with exercise. Do the “bridge” in the morning. Your muscles will be better developed and provide better support for your joints throughout the day. You can do other thigh exercises that are not contraindicated to you. Consult with your doctor.
- Put something cold on the inflamed area. The best is ice wrapped in a cloth. The cold reduces inflammation and helps relieve pain. You can do this up to 4-5 times a day for 10-15 minutes.
- Use heat for arthritis. Warming the arthritic thigh with a hot shower or bath can help relieve pain. But do not use heat for bunions. It can make the inflammation even more serious.
- Do stretching for bunions. Stretch the muscles for 30 seconds 1-3 times. Hold on to something strong to keep your balance.
- Strengthen the inner thigh muscles. Lie on your back. Place a ball (about the size of a soccer) between your knees and squeeze. Start with one set of 10 repetitions. Gradually build up to 30 reps (3×10).
- For arthritis, develop the external muscles. Lie down on your side, which does not hurt. Lift the painful leg about 15 cm. Hold for 2 to 3 seconds and then lower. Start with one approach of 10 repetitions. Gradually bring them to 3 sets of 10 repetitions. Do not perform this exercise if you have bunions.
- Exercise in water. Swimming and water aerobics are excellent methods of strengthening the muscles of the thigh without much stress on the joints.
- Avoid serious physical activity. Running and jumping can increase pain due to arthritis and bursitis. Walking is a better choice.
- Lose weight. Osteoarthritis is caused by cartilage abrasion. In this case, you need to reduce the pressure on the joint and thigh. Lose a few pounds of extra weight to reduce thigh pains.
About the Author
Reyus Mammadli is the author of this health blog since 2008. With a background in medical and biotechnical devices, he has over 15 years of experience working with medical literature and expert guidelines from WHO, CDC, Mayo Clinic, and others. His goal is to present clear, accurate health information for everyday readers — not as a substitute for medical advice.